If you run a hospital, rehab facility, or skilled nursing center, you already know that billing is half the battle. You take care of patients, but if the paperwork doesn’t follow, the money doesn’t come in. Enter the UB-04 claim form. It helps you a lot when it comes to getting paid on time and in full.
This guide unpacks everything providers need to know about the UB-04: what it is, who uses it, where it’s used, how to fill it out correctly, and why it matters.
What Is the UB-04 Claim Form?
The UB-04, also known as CMS-1450 (and previously the UB-92), is the standard claim form used by institutional providers to bill payers like Medicare, Medicaid, Tricare, commercial insurers, and even workers’ compensation. If your practice operates as a hospital, skilled nursing facility, hospice, rehab center, or ambulatory surgery center (ASC), this is your primary tool for getting paid.
In simpler terms:
- The CMS-1500 is for individual providers (think: physicians, NPs, therapists).
- The UB-04 is for institutions and facilities providing services in a clinical setting.
Quick Snapshot:
- Standardized by the National Uniform Billing Committee (NUBC)
- Accepted by all major payers
- Used for over 98% of Medicare claims
- Captures care details using ICD-10, CPT/HCPCS codes
History of UB-04 Claim Form
Back in the ’80s, we had the UB-92. It worked fine—until it didn’t. The healthcare system outgrew it, and by 2007, the UB-04 took over.
The upgrade brought:
· More form fields
· More clarity
· Better support for electronic billing
· A structure that plays nicely with modern RCM systems
Thanks to UB-04, insurance claims from hospitals are far less of a guessing game and more of a well-documented request.
CMS-1500 vs UB-04: What’s the Real Difference?
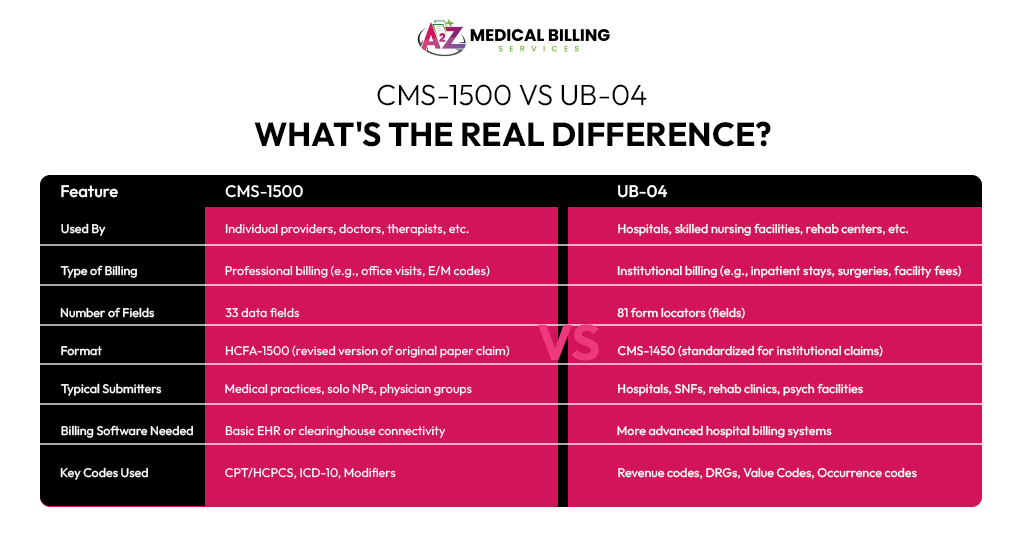
Both CMS-1500 and UB-04 are critical billing forms, but they serve different types of providers and payment workflows. Knowing which one to use—and when—can make or break your revenue cycle.
| Feature | CMS-1500 | UB-04 |
| Used By | Individual providers, doctors, therapists, etc. | Hospitals, skilled nursing facilities, rehab centers, etc. |
| Type of Billing | Professional billing (e.g., office visits, E/M codes) | Institutional billing (e.g., inpatient stays, surgeries, facility fees) |
| Number of Fields | 33 data fields | 81 form locators (fields) |
| Format | HCFA-1500 (revised version of original paper claim) | CMS-1450 (standardized for institutional claims) |
| Typical Submitters | Medical practices, solo NPs, physician groups | Hospitals, SNFs, rehab clinics, psych facilities |
| Billing Software Needed | Basic EHR or clearinghouse connectivity | More advanced hospital billing systems |
| Key Codes Used | CPT/HCPCS, ICD-10, Modifiers | Revenue codes, DRGs, Value Codes, Occurrence codes |
· Scenario 1: A dermatologist bills for a routine skin check. → CMS-1500
· Scenario 2: A hospital bills for a 2-night inpatient stay with surgery. → UB-04
Using the wrong form could lead to claim denials, delayed payments, or compliance issues. Even clearinghouses flag mismatches immediately—so train your team to get this right.
If you’re billing facility fees, use UB-04. If it’s a provider’s time or effort, use CMS-1500.
Why the UB-04 Form Matters for Providers
Let’s not sugarcoat it — billing is life or death for your revenue cycle. The UB-04 does more than ask payers for money. It:
1. Tells a clear, coded story of what happened to the patient
2. Justifies the cost of care with supporting data
3. Reduces denials due to missing or inconsistent information
4. Speeds up payments so you’re not stuck in 90-day AR cycles
5. Keeps compliance tight so you don’t risk fraud or fines
Who Uses the UB-04?
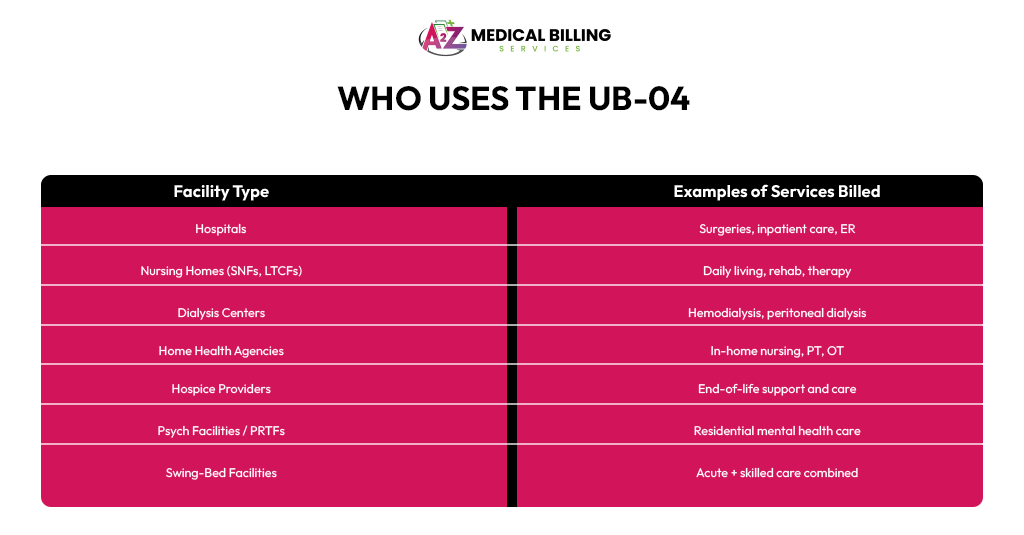
Any provider that’s part of a facility rather than a solo practice. That includes:
| Facility Type | Examples of Services Billed |
| Hospitals | Surgeries, inpatient care, ER |
| Nursing Homes (SNFs, LTCFs) | Daily living, rehab, therapy |
| Dialysis Centers | Hemodialysis, peritoneal dialysis |
| Home Health Agencies | In-home nursing, PT, OT |
| Hospice Providers | End-of-life support and care |
| Psych Facilities / PRTFs | Residential mental health care |
| Swing-Bed Facilities | Acute + skilled care combined |
Because they don’t just provide a procedure — they give an entire episode of care. The UB-04 form is built to document every aspect of that episode, from check-in to discharge.
Where Is the UB-04 Claim Form Used?
The UB-04 form isn’t exclusive to Medicare billing—it’s the industry standard for institutional claims across the entire U.S. healthcare system. Whether you’re billing for a hip replacement or hospice care, if you’re a facility, the UB-04 is your go-to form.
Here’s where and how it’s used:
Medicare & Medicaid
UB-04 is the primary claim form for billing Medicare (federal) and Medicaid (state) for inpatient and outpatient services provided to:
· Older adults (65+)
· Disabled individuals
· Low-income patients
Example: A nursing home submits a UB-04 to Medicaid for a 30-day rehab stay after a patient breaks a hip. It includes dates, treatments, therapy sessions, and medication.
Why UB-04? Because it captures the whole picture—from the room stay to the physical therapy—so CMS can adequately evaluate the claim.
Private Health Insurance Companies
Major private payers like Blue Cross Blue Shield, Aetna, UnitedHealthcare, and others also accept the UB-04 for institutional claims.
Example: A hospital bills Aetna for a patient’s outpatient colonoscopy. The UB-04 includes the procedure code, diagnosis, supplies used, and discharge time.
Why it works: The form’s coding system (ICD-10, CPT, HCPCS) ensures everyone’s on the same page—no confusion, no phone tag.
Workers’ Compensation Programs
When a worker gets injured on the job and is hospitalized or treated in an urgent care clinic, the facility uses the UB-04 to bill state workers’ comp programs.
Example: A construction worker is hospitalized for a back injury after a fall. The hospital bills the state’s workers’ compensation system using a UB-04 form detailing the ER visit, imaging, and physical therapy.
It documents exactly what was done, which supports proper reimbursement and liability review.
Military and Other Government Programs
Programs like TRICARE (military healthcare), Indian Health Services (IHS), VA programs, and state-funded initiatives also rely on the UB-04 form for facility-based claims.
Example: A TRICARE patient receives outpatient surgery at a civilian hospital. That hospital uses a UB-04 to request payment from the Department of Defense’s healthcare contractor.
These payers use UB-04 because it standardizes how they receive, review, and pay for complex institutional care.
Self-Pay Patients
Even if a patient doesn’t have insurance, your billing department may still use the UB-04 as a formal invoice or statement of charges for inpatient or outpatient services.
Example: An uninsured patient receives emergency surgery and later requests an itemized statement for their records or to apply for charity care. The hospital provides a UB-04 showing all services rendered.
Using the UB-04 for self-pay makes the billing transparent and uniform—and helps with payment plans or legal documentation.
What’s Inside the UB-04? (Key Form Locators)
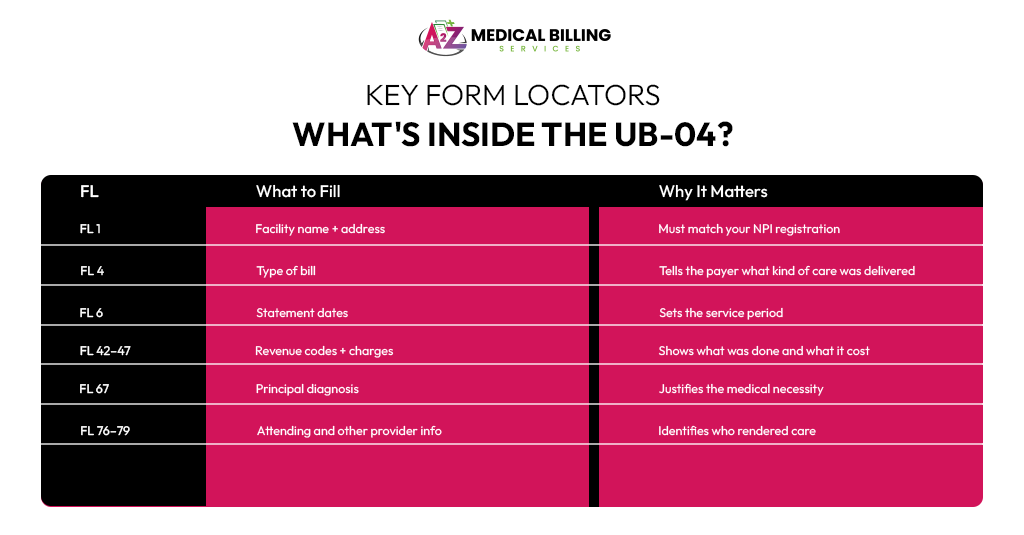
The UB-04 has 81 fields, also called Form Locators (FLs). Some are required for all claims; others depend on the situation.
Here are a few key ones:
| FL | What to Fill | Why It Matters |
| FL 1 | Facility name + address | Must match your NPI registration |
| FL 4 | Type of bill | Tells the payer what kind of care was delivered |
| FL 6 | Statement dates | Sets the service period |
| FL 42–47 | Revenue codes + charges | Shows what was done and what it cost |
| FL 67 | Principal diagnosis | Justifies the medical necessity |
| FL 76–79 | Attending and other provider info | Identifies who rendered care |
How the UB-04 Improves Revenue Cycle
The UB-04 is more than a billing form. It’s a revenue tool, a compliance shield, and a communication bridge between you and payers. If your team treats it as just another document, you’re leaving money on the table—and opening the door to denials, audits, and delays.
Here’s how this UB-04 form directly improves revenue cycle performance—and saves your facility time, money, and headaches.
Fewer Denials = Cleaner Cash Flow
Payers reject thousands of claims daily for missing or mismatched data. The standardized UB-04 helps cut through that noise.
Real example: Instead of getting denied for “incomplete diagnosis” or “missing discharge code,” your UB-04 includes every necessary field — diagnosis, NPI, service codes, charges — in a clear, payer-friendly format. It’s like handing in a perfectly filled Scantron. No one questions it.
· Reduces claim resubmissions
· Lowers admin overhead
· Speeds up payment cycles
Faster Reimbursements
The longer you wait for a payer to process a claim, the older your accounts receivable will become—and aged AR = unpaid bills, unhappy CFO.
The UB-04’s clarity minimizes delays caused by back-and-forth emails or payer requests for clarification.
Your billing team submits a UB-04 to Medicare for a 5-day inpatient stay with supporting codes for labs, imaging, and therapy. Because all boxes are correctly completed, the claim clears without interruption—and the payment hits your account in under 15 days.
When your revenue comes in faster, you can reinvest sooner — in staffing, technology, or even snacks in the breakroom.
Cleaner Audits = Fewer Sleepless Nights
When CMS or a commercial payer audits your claims, they’re looking for accuracy, consistency, and compliance.
The UB-04, when filled correctly, becomes your defense against recoupments and legal trouble. It shows who delivered care, what they did, and why it was necessary — all in one form.
For example, in a post-payment audit, your facility is asked to justify a patient’s extended rehab stay. The UB-04 reveals accurate billing dates, services performed, therapy codes, and medical necessity—making your case solid and denials unlikely.
Accurate Provider Payments
Behind every claim are real people—nurses, techs, specialists—who deserve to be paid. The UB-04 makes sure their work doesn’t get lost in the shuffle.
Because it captures every service line item, it helps your accounting team allocate revenue back to the right cost centers and providers.
Example: Your rehab department can bill for each PT session, your radiology team gets credit for scans performed, and even pharmacy charges are neatly tracked. Everyone gets paid based on clean, traceable data.
Better Compliance with CMS and Commercial Payers
Healthcare billing fraud is no joke. Penalties can include heavy fines and even criminal charges. But honest mistakes can still trigger red flags if your billing isn’t airtight.
The UB-04 keeps you compliant by forcing standardized, traceable, verifiable reporting.
· Reduces risk of False Claims Act violations
· Ensures accurate NPI use
· Documents medical necessity with proper codes
It’s your safeguard against unintentional non-compliance.
Final Thoughts
The UB-04 may be decades old, but it’s still the backbone of facility billing in America. Whether you’re submitting claims to Medicare, Medicaid, TRICARE, or private payers, this form helps hospitals, SNFs, and other institutional providers get paid correctly and on time.
If you’re a biller, coder, or provider, don’t treat the UB-04 like just another form. Master it. Understand what each field does. Because every box, every digit, every modifier can make the difference between payment and denial, between compliance and audit trouble.
In short: The UB-04 isn’t going anywhere—so the smarter you work with it, the more efficient your revenue cycle becomes.
Frequently Asked Questions (FAQs)
Who fills out the UB-04 form?
Typically, billing departments, medical billers, or revenue cycle staff fill out the UB-04. In smaller practices or facilities, certified coders or practice managers may also handle it.
Can physicians use the UB-04 form?
No. Physicians and non-institutional providers use the CMS-1500 form. UB-04 is only for institutional providers like hospitals, rehab centers, SNFs, and some outpatient clinics.
What happens if I submit a UB-04 with errors?
You risk delayed payments, denials, or audits. Even small mistakes like incorrect condition codes or missing provider numbers can cause issues with CMS or commercial payers.
Is the UB-04 used for telehealth?
Yes, but only when institutional providers bill for telehealth services. You’ll need to include specific revenue codes and modifiers that indicate the service was delivered remotely.
How often does the UB-04 get updated?
While the form itself doesn’t change often, the coding standards (like revenue codes, condition codes, etc.) are regularly updated—usually by the National Uniform Billing Committee (NUBC) or CMS.
Can I submit the UB-04 electronically?
Yes! Most providers now submit UB-04 data electronically using the 837I (Institutional) format. Paper UB-04s are still accepted but less common.
What’s the biggest mistake billers make with the UB-04?
Missing or incorrect Value Codes, Condition Codes, or Patient Status fields. These are essential for both payer rules and reimbursement logic.



