Mental health care has finally taken center stage. More Americans are seeing therapists, counselors, and psychiatrists than ever before, but the real struggle isn’t just finding the right provider—it’s figuring out how much insurance will pay.
Blue Cross Blue Shield (BCBS), with its numerous state affiliates, covers nearly one in three Americans. That’s massive. Yet if you call three BCBS members in three states, you’ll get three completely different answers on reimbursement rates for therapy.
Patients want to know: “How much will I owe out-of-pocket?”
Providers want to know: “How much will I get paid per session?”
This blog clears the fog. We’ll delve into the differences between in-network and out-of-network reimbursement, CPT codes, BCBS plan types, state-specific variations, payer-specific nuances, billing processes, and real-world scenarios.
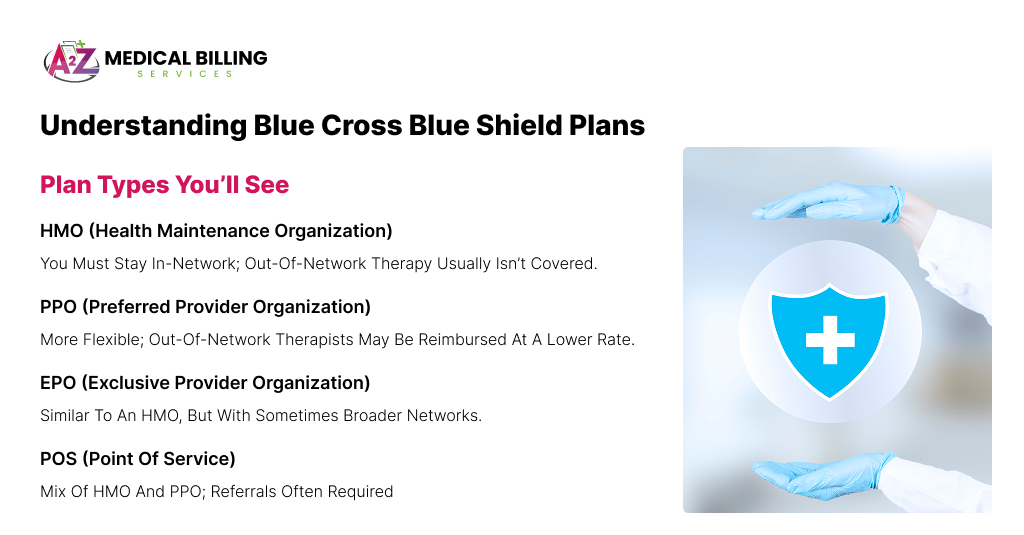
Understanding Blue Cross Blue Shield Plans
First, let’s set the stage. Blue Cross Blue Shield isn’t a single company. It’s a federation of 33 independent companies serving different states (think BCBS Texas, BCBS Illinois, BCBS Massachusetts). That’s why reimbursement rates aren’t uniform; they’re negotiated locally.
Plan Types You’ll See
- HMO (Health Maintenance Organization): You must stay in-network; out-of-network therapy usually isn’t covered.
- PPO (Preferred Provider Organization): More flexible; out-of-network therapists may be reimbursed at a lower rate.
- EPO (Exclusive Provider Organization): Similar to an HMO, but with sometimes broader networks.
- POS (Point of Service): Mix of HMO and PPO; referrals often required.
The type of plan heavily dictates how much BCBS reimburses for therapy. PPO = more flexibility, but usually higher costs for patients.
In-Network vs. Out-of-Network Therapy
This is the heart of confusion.
In-Network Therapy
- Provider has a contract with BCBS.
- Reimbursement rates are pre-negotiated and fixed.
- The patient typically pays a copay ($15–$50 per session) or coinsurance after meeting the deductible.
- Example: A 60-minute therapy session (CPT 90837) might cost $160, but in-network BCBS will pay the therapist $120, and you only owe $30.
Out-of-Network Therapy
- Provider sets their own rate.
- Patient pays full cost upfront ($120–$250 is common).
- BCBS reimburses based on the UCR (Usual, Customary, Reasonable) rate for your area.
- Typically, 50–70% of the UCR is covered after the deductible is met.
- Example: Therapist charges $180. THE BCBS UCR rate is $120. Your PPO plan covers 70% of $120 ($84). You receive a reimbursement of $84, meaning you still have to pay $96 out-of-pocket.
Out-of-network reimbursement typically falls short of the provider’s full fee. Patients are left with balance bills.
The Role of CPT Codes in Reimbursement
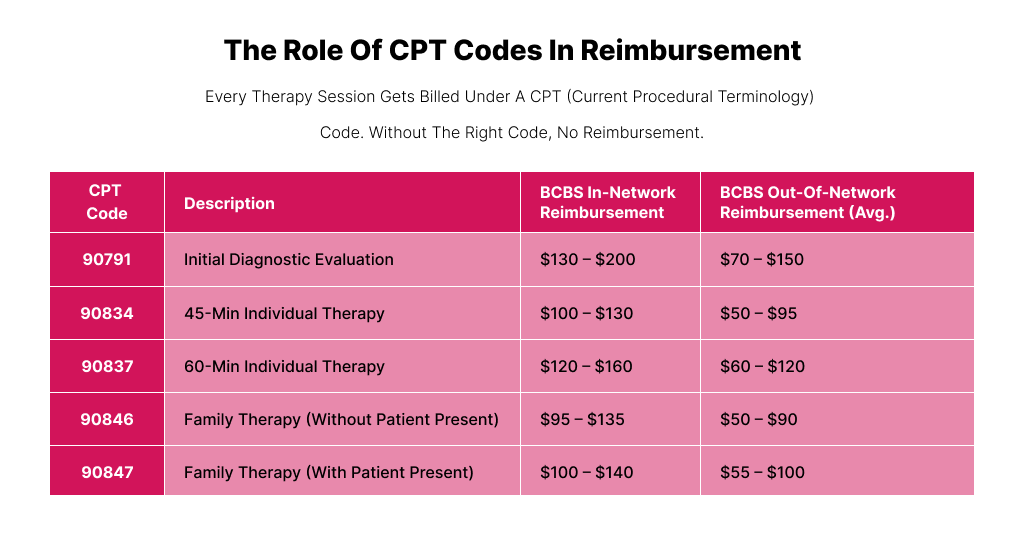
Every therapy session gets billed under a CPT (Current Procedural Terminology) code. Without the right code, no reimbursement.
Here are the heavy hitters in mental health billing:
| CPT Code | Description | BCBS In-Network Reimbursement | BCBS Out-of-Network Reimbursement (avg.) |
| 90791 | Initial Diagnostic Evaluation | $130 – $200 | $70 – $150 |
| 90834 | 45-min Individual Therapy | $100 – $130 | $50 – $95 |
| 90837 | 60-min Individual Therapy | $120 – $160 | $60 – $120 |
| 90846 | Family Therapy (without patient present) | $95 – $135 | $50 – $90 |
| 90847 | Family Therapy (with patient present) | $100 – $140 | $55 – $100 |
Tip for providers: If you’re delivering a full-hour session, bill 90837. But some insurers flag it for “overuse,” so document clearly why longer therapy was medically necessary.
How Much Does BCBS Pay by State?
Because BCBS affiliates negotiate rates separately, Alabama’s BCBS reimbursement looks different from California’s or Illinois’.
Example: CPT 90837 (60-minute Individual Therapy)
- Alabama (BCBSAL): $85–$95 in-network
- California (Blue Shield of CA): $100–$120 in-network; $80–$100 out-of-network
- Massachusetts (BCBSMA): $120–$135 in-network; telehealth reimbursed at parity with in-person
- Illinois (BCBSIL): $110–$125 in-network; out-of-network ~70% of UCR ($70–$95)
As you can see, rates fluctuate by $30–$50, depending on the location.
Medicare, Medicaid, and BCBS Commercial Plans
Since BCBS often administers Medicare Advantage and Medicaid plans in many states, let’s compare them.
Medicare (via BCBS Medicare Advantage)
- 90834 (45-min therapy): ~$80–$90
- 90837 (60-min therapy): ~$100–$120
- Patients usually pay 20% coinsurance unless they have supplemental coverage.
Medicaid (state-dependent)
- Typically lower than commercial rates.
- Many states cap 90837 at ~$60–$75.
- Some limit the number of sessions per year unless prior authorization is obtained.
Commercial BCBS Plans
- By far the most generous.
- PPO plans reimburse $100–$160 for standard sessions.
- Deductibles matter—patients often pay the full session price until the deductible is met.
The Billing Process with BCBS
Whether you’re a provider billing directly or a patient submitting a superbill, here’s the step-by-step.
- Verify Eligibility – Always call BCBS before the first session. Ask: “What’s the allowed amount for CPT 90837 under this plan?”
- Check Deductible – If the deductible isn’t met, the patient pays the full contracted rate until it is.
- Submit Claim – Providers submit claims electronically; patients use superbills if they are out-of-network.
- Reimbursement Issued – In-network: Direct payment to the provider. Out-of-network = check mailed to patient.
- Handle Denials – Common reasons: wrong CPT code, missing modifiers (telehealth often requires modifier 95), or exceeding session limits.
| Scenario 1: In-Network, Gold PPO Plan Therapist bills 90837 ($150). The BCBS rate is $125. Patient pays $20 copay. Provider gets $125. Everyone’s happy.Scenario 2: Out-of-Network, PPO Plan The therapist charges $180. BCBS UCR is $120. Plan covers 70% ($84). The patient is reimbursed $84 after meeting the deductible, with an effective out-of-pocket cost of $96.Scenario 3: HMO Plan The patient attempts to see a therapist who is out of network. Denied. Unless it’s an emergency, no reimbursement at all. |
Common Billing Mistakes That Cost Money
Even the most experienced providers make small billing mistakes that snowball into big revenue problems.
With insurers like Blue Cross Blue Shield (BCBS), errors don’t just delay payments—they can cause outright denials, lost revenue, and compliance headaches.
The key is identifying where mistakes typically occur and correcting them before claims are sent out.
Here are some of the most common errors we see:
- Submitting the wrong CPT code – Example: billing CPT 90837 (60-minute psychotherapy) when the session lasted only 45 minutes. That should be 90834, and payers like BCBS will often downcode or deny when the time doesn’t match the documentation.
- Forgetting telehealth modifiers – If you provide remote sessions and don’t include the correct modifier (95 or GT, depending on state rules), BCBS treats it as an invalid claim. One missing modifier can mean weeks of delayed cash flow.
- Using expired insurance card details – A simple oversight, such as entering an outdated policy number, results in a claim rejection. By the time you fix and resubmit, you may hit BCBS’s prompt filing limits.
- Missing prior authorization – Extended therapy sessions or intensive outpatient programs often need prior approval. Skipping this step almost guarantees a denial.
- Late submission – BCBS deadlines vary by state, but most fall between 90 and 180 days. Submitting even one day late can result in the permanent loss of payment.
Tips & Best Practices (For Providers and Patients)
Avoiding denials and maximizing reimbursement requires more than coding knowledge—it’s about following best practices at every step of the billing cycle. The good news? With a few proactive habits, providers and patients can prevent most of the problems that cause payment delays.
- Always call BCBS before the first visit. Don’t assume coverage. Ask about copays, deductibles, session limits, and whether prior authorization is needed. This protects both your revenue and your patients from surprise bills.
- Document medical necessity thoroughly. Especially for longer sessions billed under CPT 90837, BCBS reviewers want to see why a 60-minute session was required—strong documentation results in fewer audits and fewer downgrades.
- Encourage patients to file superbills. If you’re an out-of-network provider, patients can still recover partial reimbursement by submitting a superbill to BCBS. It’s a small step that builds goodwill and helps patients offset costs.
- Track and appeal denials. Don’t just write off denied claims. Many BCBS denials are overturned on appeal, especially when related to authorization or medical necessity. Keep a log of denials and check patterns.
- Watch parity laws. Many states now require BCBS and other insurers to reimburse mental health services at the same rate as physical health visits. Knowing your state’s laws can help you contest unfairly low reimbursement.
Frequently Asked Questions (FAQs)
How much does BCBS usually reimburse for a 60-minute therapy session?
Reimbursement rates vary by state, plan type, and whether your provider is in-network. On average, in-network reimbursement for CPT 90837 (a 60-minute psychotherapy session) ranges between $120 and $160 per session. If you’re an out-of-network provider, BCBS may reimburse at 50–70% of “usual, customary, and reasonable (UCR)” rates, which often comes out to $60–$120 per session.
Does BCBS cover online therapy?
Yes, most BCBS affiliates cover telehealth services, and in many states, they are required to reimburse at the same rate as in-person visits due to parity laws. If you’re planning to see a therapist online, it’s always smart to confirm coverage with BCBS before your first session.
Will BCBS reimburse if my therapist is out-of-network?
That depends on your plan type. PPO plans typically offer some out-of-network coverage, often reimbursing 50–70% of UCR rates after you have met your deductible. On the other hand, HMO and EPO plans typically don’t cover out-of-network providers at all, except in emergencies.
Do I have to meet a deductible first?
In most cases, yes. Many BCBS plans require you to meet your annual deductible before the insurer begins covering therapy sessions. Once your deductible is met, BCBS typically pays a portion of the session fee while you cover a copay or coinsurance.
Do psychiatrists receive more reimbursement than therapists?
Yes. Psychiatrists are medical doctors who can prescribe medication, so their services fall under a different reimbursement category than therapy-only visits. For example, medication management sessions (CPT 99213, 99214, 99215) often reimburse at $150–$200 or more per visit, depending on the state and the complexity of care. In contrast, therapy-only sessions (90834, 90837) usually fall in the $90–$160 range for in-network providers.
Conclusion
Blue Cross Blue Shield’s reimbursement for therapy isn’t one-size-fits-all. In-network providers typically receive $100–$160 for standard sessions, with patients paying only a $15–$50 copayment. Out-of-network reimbursement is much lower—often 50–70% of the “reasonable” rate.
The key?
Know your plan, know your codes, and verify before you sit on the couch. For providers, meticulous billing ensures a steady revenue stream. For patients, understanding coinsurance and deductibles prevents nasty surprises.
If you’re a provider tired of claim denials or struggling with revenue loss, A2Z Medical Billing Services can help. Our team of certified coders and billing experts specializes in mental health and therapy billing for BCBS and other payers. We handle eligibility checks, coding, denial management, and payment posting so that you can focus on patient care—not paperwork.
Let A2Z simplify your billing process, improve your reimbursement rates, and strengthen your bottom line.