Colonoscopy is one of the most commonly billed GI procedures in the U.S.—both for screening and diagnostic purposes. But for practices, colonoscopy billing is also one of the most error-prone areas. Why? Because coding depends on the indication (screening vs diagnostic), findings (polyps, biopsy, bleeding), and payer (Medicare vs commercial). A single misstep can turn a fully reimbursable claim into a denial or underpayment.
In this guide, we’ll break down the CPT codes 45378–45398 and Medicare HCPCS codes G0105 and G0121, explain their usage, documentation requirements, reimbursement trends, and walk you through billing best practices so your GI practice doesn’t lose revenue.
Colonoscopy CPT Codes (45378–45398) – At a Glance
These CPT codes cover diagnostic and therapeutic colonoscopy services. Here’s a quick breakdown:
- 45378 – Diagnostic colonoscopy (includes brushings or washings, if performed)
- 45379 – Colonoscopy with removal of foreign body
- 45380 – Colonoscopy with biopsy, single or multiple
- 45381 – Colonoscopy with directed submucosal injection (e.g., for tattooing or hemostasis)
- 45382 – Colonoscopy with control of bleeding (any method)
- 45384 – Colonoscopy with removal of tumor(s), polyp(s), or lesion(s) by hot biopsy forceps
- 45385 – Colonoscopy with removal of tumor(s), polyp(s), or lesion(s) by snare technique
- 45386 – Colonoscopy with dilation (balloon, bougie, etc.)
- 45388 – Colonoscopy with ablation of tumor(s), polyp(s), or lesion(s) (e.g., argon plasma coagulation)
- 45391 – Colonoscopy with endoscopic ultrasound exam
- 45392 – Colonoscopy with endoscopic ultrasound–guided needle aspiration/biopsy
- 45397 – Colonoscopy with transendoscopic stent placement
- 45398 – Colonoscopy with band ligation
Think of 45378 as the “base” code. All other codes (45379–45398) represent additional interventions performed during the same session.
Medicare HCPCS Codes – Screening Colonoscopies
Medicare doesn’t always use CPT codes for screening colonoscopies. Instead, it uses G-codes:
- G0105 – Colorectal cancer screening, colonoscopy on an individual at high risk
- G0121 – Colorectal cancer screening, colonoscopy on an individual not meeting high-risk criteria
When to use these?
- Use G0105 if the patient has a family history of colon cancer, prior polyps, or other risk factors.
- Use G0121 for average-risk patients.
If a screening colonoscopy finds and removes a polyp, you switch from a screening G-code to the appropriate CPT therapeutic code (e.g., 45385), and append modifier PT (colorectal cancer screening test converted to diagnostic test).
Documentation Requirements
To avoid denials, documentation must clearly state:
- Indication: screening vs diagnostic
- Risk status: average vs high risk (family history, past history, genetic syndrome)
- Procedure performed: biopsy, snare, stent, ablation, bleeding control, etc.
- Findings: polyps, lesions, diverticulosis, normal exam
- Interventions: specify tools (forceps, snare, APC) and method used
Pro tip: If a polyp is removed, specify how it was removed (snare vs biopsy forceps), since that determines whether you bill 45384 or 45385.
Reimbursement Rates
Reimbursement varies by payer and region, but here’s the 2025 Medicare Physician Fee Schedule (approximate national average):
- 45378 (Diagnostic colonoscopy) – $335
- 45380 (Biopsy) – $450
- 45385 (Snare polypectomy) – $500–$525
- 45398 (Band ligation) – $480
- G0105 / G0121 (Screening colonoscopy) – $330–$350
Commercial payers typically reimburse 15–30% higher than Medicare rates, but patient cost-sharing depends heavily on whether the service remains classified as “preventive” under ACA rules.
Billing Process for Colonoscopy
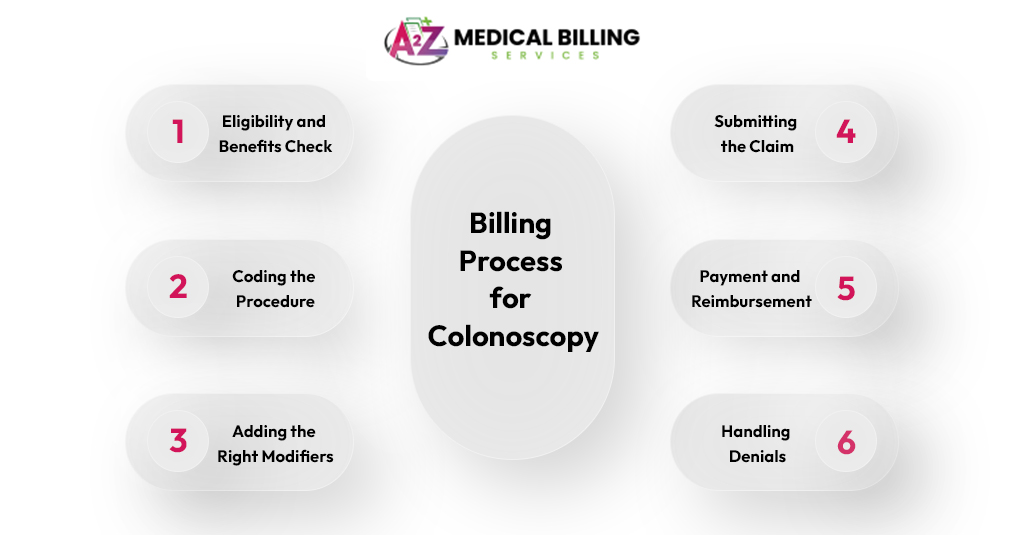
Billing for a colonoscopy isn’t just about slapping a CPT code on a claim and hitting submit. It’s a workflow that starts before the patient walks in and ends only after the payment is in your account. Here’s how the process flows:
Step 1: Eligibility and Benefits Check
It starts at scheduling or check-in. Your staff contacts the payer or uses an eligibility portal to check:
- Is the patient covered for colonoscopy?
- Will it be considered preventive (fully covered, no patient cost)?
- Or is it diagnostic (applies deductible/copay)?
For example, a 52-year-old with no symptoms usually qualifies for a screening (preventive). But if the same patient reports rectal bleeding, the plan will classify it as diagnostic. This early check prevents billing surprises later.
Step 2: Coding the Procedure
Once the physician performs the colonoscopy, the operative note decides which code to use.
- If it was purely diagnostic → 45378
- If a biopsy was taken → 45380
- If a polyp was removed by snare → 45385
- If it was Medicare and a screening → G0105 or G0121
The biller chooses the right code by matching indication + intervention. This is where accuracy matters—pick the wrong one, and you’ll either lose revenue or trigger a denial.
Step 3: Adding the Right Modifiers
Now the biller attaches modifiers so the payer knows how to process the claim.
- Modifier 33 → tells commercial plans the service is preventive.
- Modifier PT → tells Medicare the screening turned into diagnostic (like when a polyp is removed).
Without modifiers, payers often process the claim as diagnostic, and the patient gets an unexpected bill.
Step 4: Submitting the Claim
The claim goes out electronically through the clearinghouse. At this point, ICD-10 codes must back up the reason for the procedure.
- Screening codes: Z12.11 (screening for colon cancer), Z80.0 (family history).
- Diagnostic codes: K63.5 (polyp), K62.5 (rectal bleeding), R19.5 (other fecal abnormalities).
If it was a screening that found a polyp, the biller lists Z12.11 first, then adds K63.5. This makes it clear the exam started as preventive but had findings.
Step 5: Payment and Reimbursement
Once processed, the payer reimburses based on fee schedules. Medicare pays around $330–$525, depending on the code. Commercial payers usually pay a little more, depending on contracts.
The biller posts the payment, checks it against the expected rate, and flags any underpayments. Practices that skip this step often leave money uncollected without realizing it.
Step 6: Handling Denials
If the payer denies the claim, it goes into denial management. Colonoscopy denials usually happen because:
- The wrong screening/diagnostic code was used.
- The required modifier wasn’t added.
- ICD-10 didn’t support medical necessity.
- Bundled services were billed separately.
The billing team corrects the error, resubmits, and updates workflow to prevent the same issue in the future.
Common Colonoscopy Claim Denials and How They Work
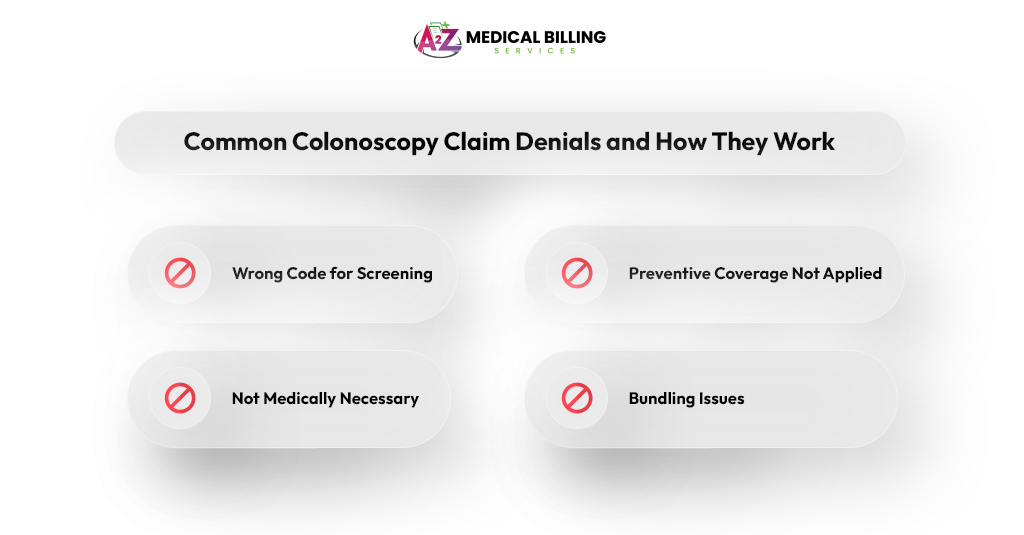
Colonoscopy claims are some of the most frequently denied in GI billing. The reasons usually fall into four predictable buckets. Here’s what happens and how to avoid it:
Denied: Wrong Code for Screening
Medicare doesn’t use CPT codes for screening colonoscopies. If you bill a screening as 45378 instead of G0105 (high risk) or G0121 (average risk), Medicare automatically denies the claim.
How to avoid it:
- Always use G-codes for Medicare patients.
- Save CPT codes for commercial insurance.
- Train schedulers and billers to flag Medicare patients upfront so the right code is applied from the start.
Denied: Preventive Coverage Not Applied
Even if the procedure was preventive, the payer processes it as diagnostic because no modifier was added. The claim gets paid, but the patient ends up with a bill for their deductible or copay. This usually leads to angry phone calls.
How to avoid it:
- For commercial payers, add modifier 33 to tell them it’s preventive.
- For Medicare, add modifier PT when a screening turns diagnostic (like finding and removing a polyp).
- Make modifier use a mandatory checklist item before claim submission.
Denied: Not Medically Necessary
The payer says there’s no valid reason to cover the procedure based on the diagnosis code you used. For example, if you bill 45380 (colonoscopy with biopsy) but only list Z12.11 (screening) as the diagnosis, the payer thinks there was no medical need for the biopsy.
How to avoid it:
- Use Z-codes for screening (Z12.11 for colon cancer screening, Z80.0 for family history).
- Add condition-specific codes when findings occur (K63.5 for polyp, K62.5 for bleeding).
- Always code the reason for the procedure and the findings.
4. Denied: Bundling Issues
Some colonoscopy codes are considered bundled—meaning you can’t bill them together. For example, if you bill 45378 (diagnostic colonoscopy) and 45385 (snare polypectomy) on the same claim, the payer will deny one because the diagnostic portion is already included in the therapeutic code.
How to avoid it:
- Know which CPT codes are mutually exclusive.
- Bill only the highest-level therapeutic service performed.
- Use modifier 59 only if two distinct procedures were done at separate sites, not as a blanket fix.
Pro Tips for Providers
- Always differentiate screening vs diagnostic up front when scheduling and coding.
- Educate staff on Medicare’s G0105/G0121 requirements.
- Document polyp removal techniques precisely.
- Use modifier 59 only if two distinct procedures were performed in separate anatomical sites.
- Run regular denial audits—colonoscopies are among the top 10 most denied GI services.
- Post clear financial counseling for patients so they aren’t surprised by bills if a “screening” turns into “diagnostic.”
Conclusion
Colonoscopy billing looks straightforward until you add in modifiers, Medicare G-codes, and the screening-to-diagnostic switch. Practices that stay on top of documentation, payer rules, and coding distinctions see faster payments and fewer denials.
If your practice struggles with GI billing complexities, outsourcing colonoscopy billing to experts can save 15–20% in lost revenue annually.
A2Z Medical Billing Solutions specializes in colonoscopy and gastroenterology billing. From eligibility verification to denial management, we ensure your claims are paid right—the first time. Contact us today to optimize your revenue cycle.



