Medical billing becomes challenging, especially when CPT coding rules come into play. One of the most common areas of confusion for providers is the difference between timed and untimed CPT codes. At first glance, the distinction may seem simple. However, in real-world billing, small misunderstandings around time, units, and documentation can quickly turn into denied claims, delayed payments, or compliance risks. This guide clearly and practically breaks down timed versus untimed CPT codes. It explains how each code type works, how to bill them correctly, and what providers must do to stay compliant while protecting reimbursement.
What Are CPT Codes?
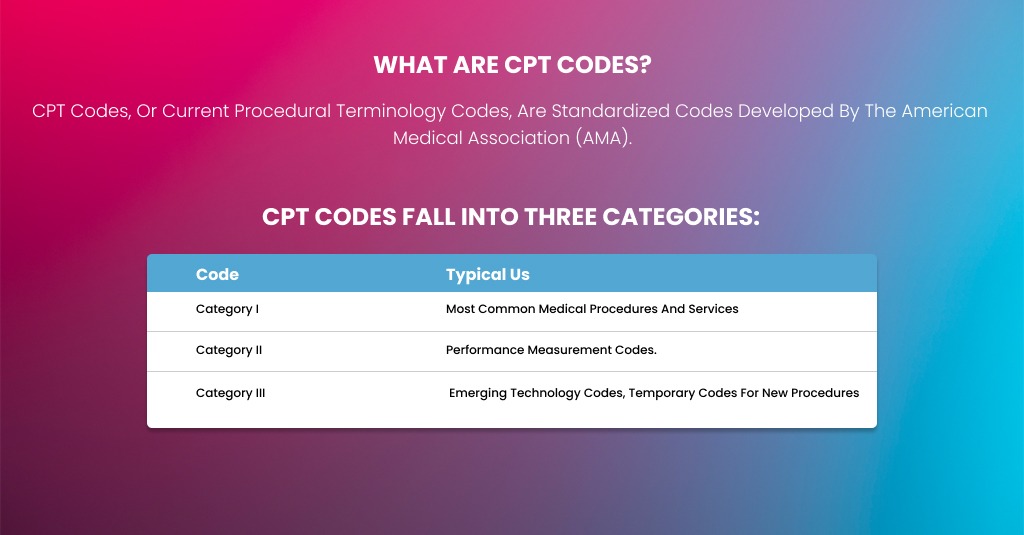
CPT codes, or Current Procedural Terminology codes, are standardized codes developed by the American Medical Association (AMA) to describe medical, surgical, and diagnostic procedures. They are used by providers, insurers, and government programs to ensure uniform billing and documentation.
CPT codes fall into three categories:
- Category I: Most common medical procedures and services.
- Category II: Performance measurement codes.
- Category III: Emerging technology codes, temporary codes for new procedures.
For billing purposes, the most relevant distinction is whether a CPT code is timed or untimed. Understanding this distinction ensures providers are reimbursed correctly and avoid compliance risks.
Timed CPT Codes
Timed CPT codes are those in which reimbursement is based on the actual time a service is performed. They often apply to services such as evaluation and management (E/M), psychotherapy, physical therapy, occupational therapy, and specific procedures that require hands-on time with a patient.
Key Features of Timed Codes include:
- Time-Based Calculation: Payment depends on the number of minutes spent providing the service.
- Incremental Billing: Some timed codes allow additional units for extra time beyond the initial period.
- Documentation Required: Providers must document the start and end times, or the total duration, of the service.
Examples include:
- 90837: Psychotherapy, 60 minutes with patient and/or family
- 97110: Therapeutic exercises, every 15 minutes
- 99214: Office or other outpatient E/M visit, typically 25 minutes
Here’s a comparison table for Timed Vs Untimed CPT Codes:
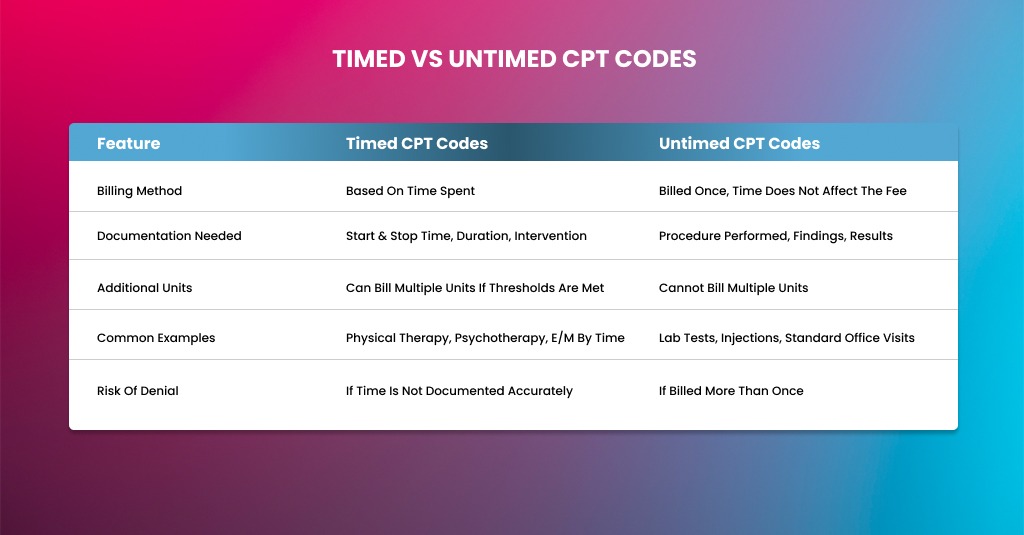
| Feature | Timed CPT Codes | Untimed CPT Codes |
| Billing Method | Based on time spent | Billed once, time does not affect the fee |
| Documentation Needed | Start & stop time, duration, intervention | Procedure performed, findings, results |
| Additional Units | Can bill multiple units if thresholds are met | Cannot bill multiple units |
| Common Examples | Physical therapy, psychotherapy, E/M by time | Lab tests, injections, standard office visits |
| Risk of Denial | If time is not documented accurately | If billed more than once |
Billing Guidelines for Timed Codes
Billing timed CPT codes requires precision. Time is the foundation of reimbursement, so even small mistakes can lead to denials or audits. Providers must follow strict documentation and calculation rules to stay compliant.
Understand What Counts as Billable Time
Not every minute spent around a patient counts as billable time. Only direct, face-to-face time or time explicitly allowed by payer rules qualifies.
Billable time usually includes:
- Direct patient interaction
- Hands-on treatment or therapy
- Counseling or coordination when permitted
- Medically necessary services tied to the CPT description
Non-billable time usually includes:
- Charting after the visit
- Waiting time
- Room setup or cleanup
- Conversations unrelated to care
Always link time to medical necessity. Time alone never justifies billing.
Follow the CPT Time Threshold Rules
Most timed CPT codes follow defined time thresholds. Providers must meet the minimum time requirement before billing even one unit.
For therapy codes billed in 15-minute increments:
- 8–22 minutes = 1 unit
- 23–37 minutes = 2 units
- 38–52 minutes = 3 units
- 53–67 minutes = 4 units
This rule applies unless a payer states otherwise. Never round up time. If the minimum threshold is not met, do not bill the unit.
Document Start and End Times Clearly
Documentation is your first line of defense in an audit. Payers expect clarity.
Your record should include:
- Start time of the service
- End time of the service
- Total time spent
- Specific interventions performed
- Patient response or progress
Avoid vague phrases like “session lasted 30 minutes.” Always show how the time was used.
Use Correct Units and Modifiers
Only bill the number of units supported by documented time. Billing extra units without time support is a common audit trigger.
Also:
- Use therapy modifiers when required
- Apply multiple procedure modifiers correctly
- Follow payer-specific unit caps per day
Incorrect unit reporting is one of the top reasons for denial of timed services.
Payer Rules Matter More Than CPT Alone
Medicare, Medicaid, and commercial payers may interpret timed codes differently.
- Medicare strictly enforces time thresholds and documentation
- Medicaid rules vary by state and often limit daily units
- Commercial payers may require prior authorization or cap sessions
Always check the payer’s policy before billing.
Untimed CPT Codes
Untimed CPT codes are billed once, regardless of how long it takes to perform the service. They are common for procedures that have a defined scope, diagnostic tests, or visits where time is not the primary factor in complexity.
Key Features of Untimed Codes are:
- Flat Fee: Payment is the same whether the procedure takes 5 minutes or 50 minutes.
- Performed Once: Typically billed once per session or per encounter.
- Documentation Still Required: Document the procedure or service performed and the patient outcome.
Examples:
- 93000: Electrocardiogram with interpretation
- 36415: Collection of venous blood by venipuncture
- 99203: N033ew patient office visit (office E/M where time is not used for billing)
Billing Guidelines for Untimed CPT Codes
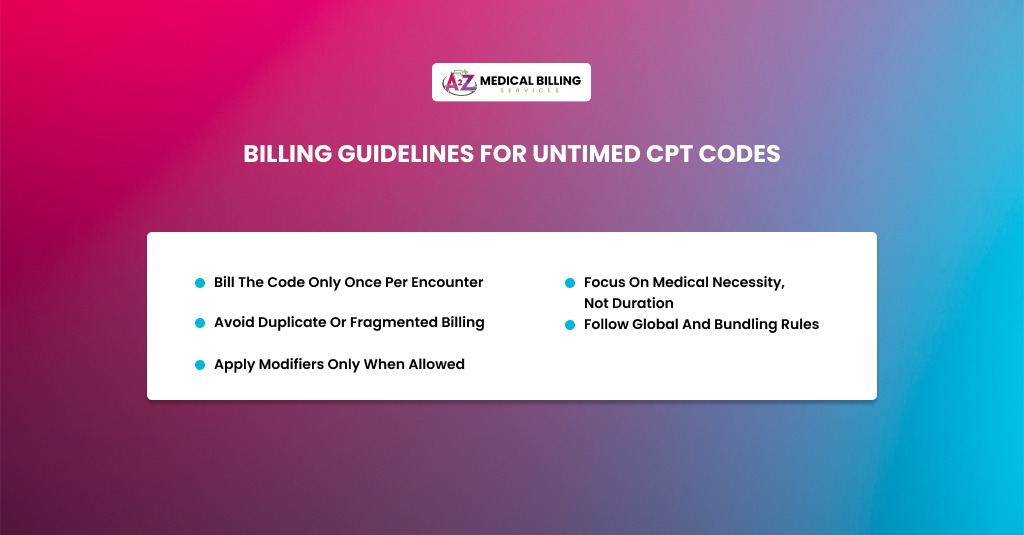
Untimed CPT codes follow a different logic. Time does not affect payment, but documentation and medical necessity still matter.
Bill the Code Only Once Per Encounter
Untimed CPT codes are billed once per session, regardless of the service’s duration.
Common examples include:
- Diagnostic tests
- Injections
- Lab draws
- Specific evaluation and management services
Do not split untimed services into multiple units. Doing so almost always leads to denials or recoupments.
Focus on Medical Necessity, Not Duration
For untimed codes, payers care more about why the service was performed than how long it took.
Your documentation should clearly explain:
- The clinical reason for the service
- Relevant patient history
- Findings or results
- Interpretation, if applicable
Even if the service took longer than usual, time does not justify higher billing.
Avoid Duplicate or Fragmented Billing
A common error with untimed codes is billing the same service more than once on the same date.
Avoid:
- Billing the same CPT code multiple times
- Separating components that are bundled
- Billing services are already included in a global package
Bundling rules apply heavily to untimed codes.
Follow Global and Bundling Rules
Many untimed CPT codes fall under:
- Global surgical packages
- Diagnostic bundling edits
- National Correct Coding Initiative rules
If a service is bundled, it cannot be billed separately unless a modifier is allowed and properly justified.
Apply Modifiers Only When Allowed
Modifiers for untimed codes must be used carefully.
Use them only when:
- The service is truly distinct
- Documentation supports separation
- Payer policy allows modifier usage
Improper modifier use is a frequent audit risk.
Common Billing Errors and How to Avoid Them
Billing errors involving timed and untimed CPT codes occur more often than most providers expect. These mistakes usually do not happen intentionally. They occur because of workflow gaps, documentation habits, or misunderstandings of payer rules. Over time, even small errors can lead to denied claims, delayed payments, or audit exposure. Understanding these errors helps providers protect revenue and maintain compliance.
Timed CPT Code Billing Errors
Timed CPT codes rely on accurate time tracking. When time documentation fails, the entire claim becomes vulnerable. Below are the most common errors providers face with timed services and how to prevent them.
Not Recording Time Properly
This is one of the most frequent causes of denied timed-code claims. Providers often document the service but fail to show the time spent clearly.
Common issues include:
- No start time or end time recorded
- Total time listed without showing how it was used
- Vague wording like “session completed” without duration
Payers, especially Medicare, expect clear time-based documentation. Without it, they may assume the service does not meet billing thresholds.
How to avoid it:
- Always record start and stop times in the medical record
- Document total minutes spent on each timed service
- Link time to the specific intervention provided
Clear time documentation protects both reimbursement and compliance.
Rounding Up Incorrectly
Rounding time up to bill extra units is a common but risky mistake. Providers may feel that a few extra minutes warrant another unit, but most payers do not allow it.
For example:
- Billing two 15-minute units for only 22 minutes of service
- Rounding 28 minutes up to 30 minutes to meet a higher threshold
Payers apply strict time thresholds. If the minimum required time is not met, the unit is not billable.
How to avoid it:
- Follow CPT and payer-specific time thresholds exactly
- Never estimate or round up time
- Use standard time calculation charts for therapy codes
Accurate time math keeps claims defensible.
Double Billing Timed Services
Double-billing occurs when providers submit multiple units for a service performed only once, or when overlapping services are billed incorrectly.
Examples include:
- Billing the same timed CPT code twice for the same session
- Billing overlapping timed services without proper separation
- Billing both individual and group therapy for the same time period
These errors often trigger audits because they inflate billed time beyond what is realistically possible.
How to avoid it:
- Ensure timed services do not overlap unless allowed
- Bill only one service per time segment
- Review daily time totals to confirm accuracy
Consistency between time, services, and units is essential.
Untimed CPT Code Billing Errors
Untimed CPT codes may seem simpler, but they carry risks of their own. These errors usually stem from a misunderstanding of how flat-fee services should be billed.
Billing Untimed Codes Multiple Times
Untimed CPT codes are billed once per encounter, regardless of duration. Billing them more than once is a common and costly error.
Examples include:
- Billing the same injection code twice on the same day
- Submitting duplicate diagnostic procedure codes
- Charging separately for components that are already included
Payers often deny or recoup these claims during post-payment reviews.
How to avoid it:
- Confirm the CPT code is truly untimed
- Bill the service only once per visit
- Review bundling rules before submitting claims
One service equals one charge.
Mistaking Timed Services for Untimed Services
This error occurs when providers treat a timed service like a flat-fee service or treat an untimed service as time-based.
Examples include:
- Billing therapy services once without considering time units
- Billing diagnostic services per minute instead of once
- Using incorrect CPT code types for similar services
This mismatch leads to underbilling or overbilling, both of which create problems.
How to avoid it:
- Verify whether the CPT code is timed or untimed before billing
- Train staff to recognize time-based services
- Use EHR prompts or billing checks to flag mismatches
Incomplete Documentation
Even though untimed codes do not require time tracking, documentation is still critical. Missing or weak documentation can result in denials.
Common gaps include:
- No description of the procedure performed
- Missing findings or results
- Lack of interpretation for diagnostic services
Without clear documentation, payers may question medical necessity.
How to avoid it:
- Clearly document the service provided
- Include findings, results, or outcomes
- Ensure the record supports why the service was necessary
Strong documentation supports every claim.
Conclusion
Understanding timed and untimed CPT codes is not just a billing technicality. It directly impacts revenue, compliance, and the practice’s overall financial health. Timed CPT codes demand accurate time tracking, proper unit calculation, and detailed documentation that clearly supports medical necessity. Untimed CPT codes, while simpler on the surface, still require strong documentation, proper bundling, and careful modifier use to avoid duplicate billing or denials.
When providers rely solely on CPT definitions without considering payer-specific rules, billing risks increase. Medicare, Medicaid, and commercial insurers all apply their own interpretations, making education and consistency essential. Regular internal audits, staff training, and standardized documentation workflows help catch errors early and keep claims clean. By applying the proper billing guidelines for both timed and untimed services, providers can reduce audit exposure, improve cash flow, and focus more confidently on patient care rather than payment issues.
Maximize Your Revenue, Minimize Billing Errors
Stop losing money to coding mistakes. A2Z Medical Billing Services ensures timed and untimed CPT codes are billed accurately, with proper documentation and payer compliance.
We handle:
- Accurate time tracking and unit calculation
- Correct billing for untimed services
- Payer-specific rules and modifiers
Focus on patient care—let us streamline your billing and get your claims paid right the first time.
Contact Our Expert Medical Coder
FAQs
What is the main difference between timed and untimed CPT codes?
The key difference lies in how services are billed. Timed CPT codes are reimbursed based on the amount of time spent providing the service. Untimed CPT codes are billed once per encounter, regardless of the service’s duration. Understanding this distinction helps providers apply the correct units, avoid overbilling, and meet payer documentation expectations.
Do all timed CPT codes require start and stop times?
Most payers expect clear time documentation for timed CPT codes, especially Medicare. While some commercial payers may accept total time documentation, start and stop times provide stronger audit protection. Clear time tracking ensures billed units match the actual service provided and reduces the risk of denials.
Can documentation alone justify billing additional timed units?
No. Documentation must support both medical necessity and the required time thresholds. Even detailed notes cannot justify billing extra units if the minimum time requirement is not met. Time, service description, and medical necessity must all align for the claim to be defensible.
Are untimed CPT codes ever allowed to be billed more than once?
In most cases, untimed CPT codes are billed once per encounter. However, limited exceptions may exist based on payer policy or medical necessity. When multiple services appear similar, modifiers and documentation must clearly show that services were separate and distinct. Without payer approval, billing untimed codes multiple times often leads to denials or recoupments.
How do modifiers impact timed and untimed CPT code billing?
Modifiers play a critical role in both code types. For timed codes, modifiers may identify therapy disciplines or distinct services. For untimed codes, modifiers are often used to bypass bundling edits or global package rules. Incorrect modifier use is a common audit trigger, so modifiers should only be applied when documentation fully supports their use.