Group psychotherapy has become a core part of behavioral health treatment across the U.S. healthcare system. It improves access to care, reduces isolation, and helps practices manage growing patient demand without sacrificing clinical quality. CPT code 90853 supports this model. Yet, it is also one of the most misunderstood and misbilled psychotherapy codes.
Group therapy programs clinically succeed but financially struggle because of weak billing workflows. Claims denied. Payments reduced. Audits triggered. Almost all of it was preventable.
This billing guide explains CPT 90853 the way payers see it. Not just the definition, but how to bill it correctly, what documentation must show, how reimbursement works, and which errors quietly drain revenue. Everything here reflects real billing and RCM experience in U.S. behavioral health practices.
What Is CPT Code 90853?
CPT code 90853 represents group psychotherapy. It is used when one or more patients participate in a structured psychotherapy session led by a qualified mental health provider.
Unlike individual or family therapy, the therapeutic work in group psychotherapy happens through shared interaction, guided discussion, and clinician-led interventions. Each patient receives treatment for their own diagnosis within the group setting.
The group must involve multiple patients. Billing 90853 for a single patient session is not allowed.
This code is not time-based in the same strict way as individual psychotherapy codes, but sessions typically last 45 to 60 minutes, depending on clinical need and payer expectations.
Why CPT 90853 Is Important in Modern Behavioral Health
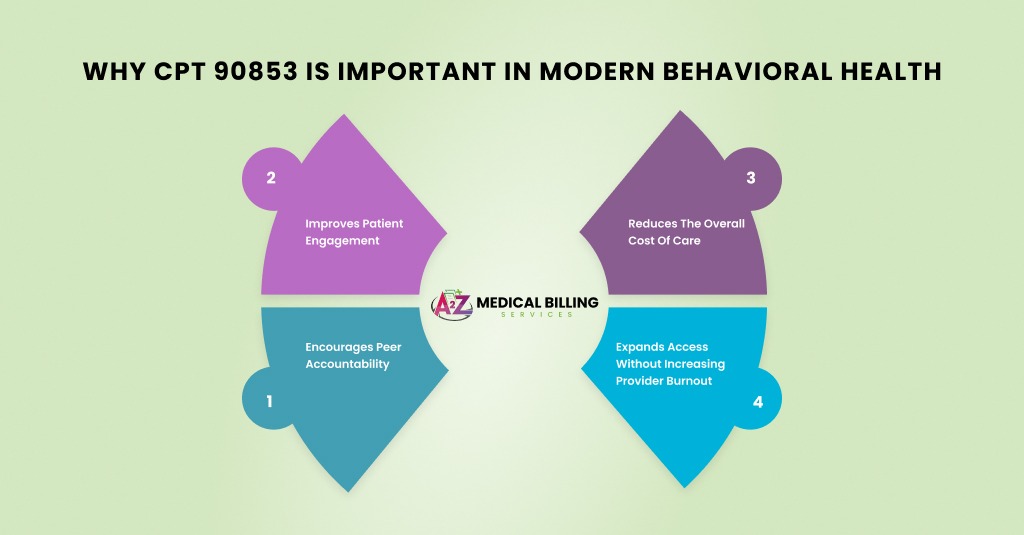
Group therapy is no longer considered secondary care. It is a frontline treatment for many conditions.
Payers support CPT 90853 because group therapy:
- Improves patient engagement
- Encourages peer accountability
- Reduces the overall cost of care
- Expands access without increasing provider burnout
From a revenue standpoint, group therapy enables practices to serve multiple patients in a single session. But that efficiency comes with higher scrutiny. Payers review group therapy claims closely to ensure services meet psychotherapy standards.
What Qualifies as Group Psychotherapy Under 90853?
Not every group session qualifies for CPT 90853.
To bill this code correctly:
- A licensed or credentialed provider must lead the session
- The session must involve active psychotherapy, not education alone
- Each patient must have a diagnosed mental health condition
- Treatment must align with each patient’s plan of care
Support groups, peer-led meetings, or educational classes do not qualify. Payers draw a clear line between psychotherapy and general group interaction.
Clinical Conditions Treated with CPT 90853
Group psychotherapy is commonly used for:
- Depression and mood disorders
- Anxiety and panic disorders
- PTSD and trauma-related conditions
- Substance use disorders
- Eating disorders
- Grief and adjustment disorders
- Anger management and emotional regulation
Each patient in the group must have a documented diagnosis. The group may be diagnosis-specific or mixed, depending on clinical design and payer rules.
How CPT 90853 Differs from Other Psychotherapy Codes
Understanding the differences prevents costly mistakes.
- 90853 vs Individual Therapy (90834/90837): 90853 treats multiple patients simultaneously. Individual therapy treats one patient at a time. You cannot bill both for the same time period.
- 90853 vs Family Therapy (90847): 90853 involves multiple patients. 90847 focuses on one identified patient with family members present.
- 90853 vs Psychoeducation Codes: Educational or skills-based groups without psychotherapy do not qualify for 90853, even if clinically valuable.
Medical Necessity for Group Psychotherapy
Medical necessity is not optional for CPT 90853.
Payers expect documentation showing:
- Why is group therapy appropriate for the patient
- How the group format supports treatment goals
- Why is individual therapy alone insufficient or supplemented
Generic statements like “group participation is beneficial” are weak. Strong documentation explains how peer interaction addresses symptoms, builds coping skills, or supports recovery.
Session Structure and Clinical Expectations
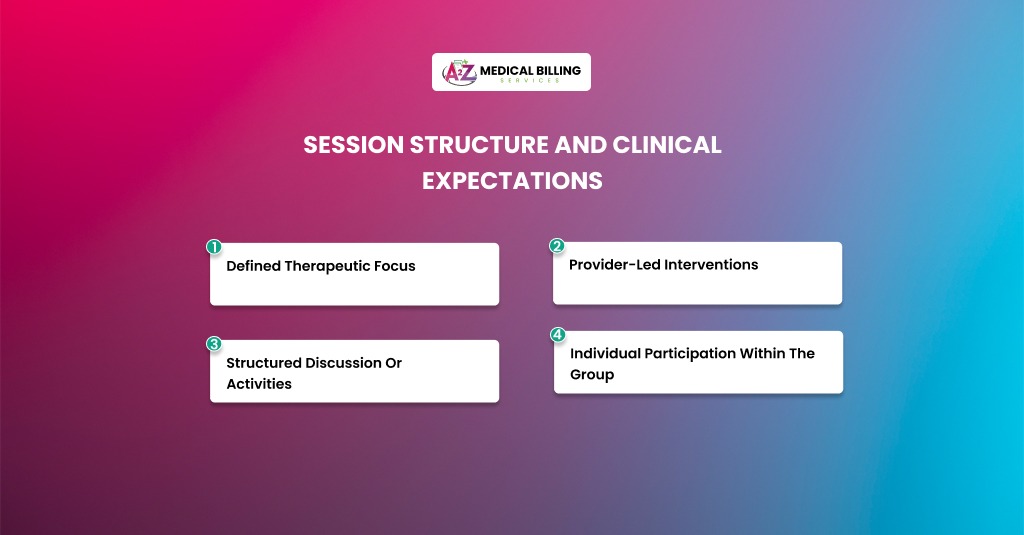
A typical CPT 90853 session includes:
- Defined therapeutic focus
- Provider-led interventions
- Structured discussion or activities
- Individual participation within the group
The provider must actively guide the session. Passive observation does not meet the standards of psychotherapy.
Documentation should reflect clinical leadership, not just attendance.
How to Bill CPT Code 90853 – Step-by-Step Billing Process
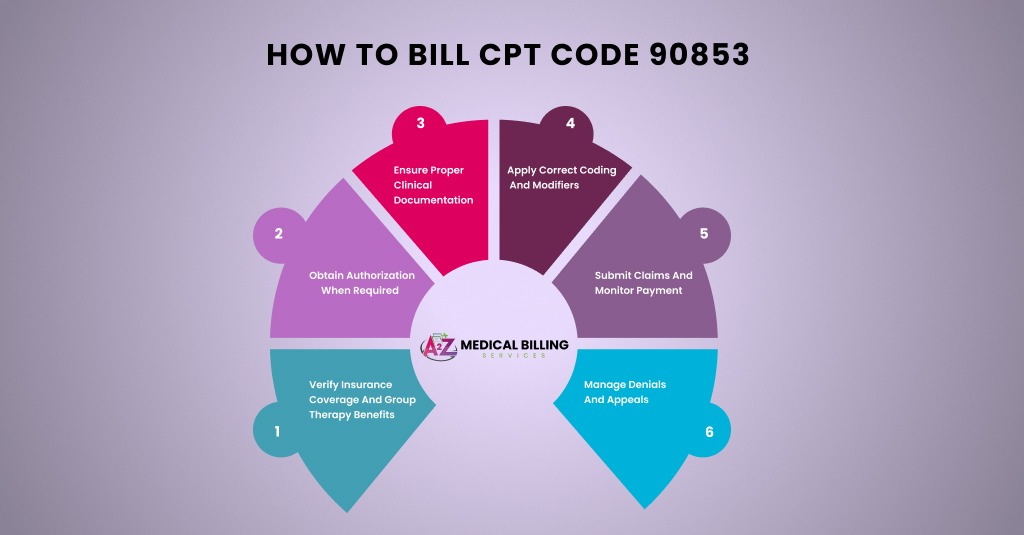
Billing CPT 90853 successfully requires coordination between the front desk, clinicians, and billing teams.
Step 1: Verify Insurance Coverage and Group Therapy Benefits
Before enrollment, verify that the patient’s plan covers group psychotherapy. Some plans limit group sessions or require prior authorization.
Confirm:
- Behavioral health benefits
- Group therapy coverage
- Visit limits
- Authorization requirements
Failure here leads to unpaid services.
Step 2: Obtain Authorization When Required
Many commercial and Medicaid plans require authorization for group therapy.
Authorization must include:
- CPT 90853
- The patient’s diagnosis
- Approved number of sessions
Using individual therapy authorization for group sessions often results in denials.
Step 3: Ensure Proper Clinical Documentation
Documentation must be individualized, even though care is delivered in a group.
Each patient’s note should include:
- Group topic and therapeutic focus
- Patient participation level
- Symptoms addressed
- Interventions applied
- Progress toward treatment goals
Copying and pasting notes across patients is a major audit trigger.
Step 4: Apply Correct Coding and Modifiers
Bill CPT 90853 for each patient who attended and participated.
Include:
- Patient-specific diagnosis code
- Rendering provider NPI
- Correct place of service
- Telehealth modifiers, if applicable
Each patient generates a separate claim line.
Step 5: Submit Claims and Monitor Payment
Group therapy claims should be tracked closely.
Monitor:
- Denials
- Reduced payments
- Visit count exhaustion
Group therapy revenue leaks often go unnoticed because volumes are high and individual payments are smaller.
Step 6: Manage Denials and Appeals
If denied, appeal with:
- Individual session notes
- Treatment plans
- Medical necessity explanation
- Authorization records
Well-supported appeals often succeed.
Reimbursement for CPT 90853
Reimbursement for CPT 90853 is lower per patient than individual therapy, but revenue scales with attendance.
Average reimbursement often ranges between $30 to $70 per patient per session, depending on payer and contract terms.
Medicare reimbursement tends to be consistent but conservative. Commercial payers vary widely.
Common Billing Errors with CPT 90853 and How to Avoid Them
A Deep-Dive Explanation from a Billing and Compliance Standpoint
Group psychotherapy billing looks simple on the surface. One provider. Multiple patients. One CPT code. In reality, CPT 90853 is one of the most audited behavioral health codes because it is easy to misuse without realizing it.
Most denials do not happen because therapy was inappropriate. They happen because payers apply very strict definitions of psychotherapy, documentation standards, and authorization rules that many practices overlook.
Let’s break down the most common billing errors in detail and, more importantly, how to fix them at the system level.
Billing Educational or Support Groups as CPT 90853
This is the number one reason group therapy claims get denied or recouped.
Payers clearly distinguish between psychotherapy and education or support. Even if a group is clinically helpful, it is not billable under CPT 90853 unless active psychotherapy is provided.
Educational groups focus on teaching information. Support groups focus on sharing experiences. Psychotherapy focuses on the clinical treatment of mental health symptoms using therapeutic techniques.
Many practices unknowingly cross this line. For example, relapse prevention education, coping skills lectures, or peer-sharing sessions without therapist-led interventions often get billed as 90853. Payers review these notes and deny them as non-covered services.
Payers look for evidence of:
- Clinical assessment during the session
- Therapeutic techniques applied
- Symptom-focused interventions
- Provider-led psychotherapy
If documentation reads like a class, workshop, or open discussion, the claim fails.
The solution is not changing the group. It is changing how the session is structured and documented.
The provider must actively guide the session, intervene therapeutically, and link discussion back to treatment goals. Documentation should describe the therapy performed, not just the topic discussed.
Instead of documenting “coping skills reviewed,” document how the provider used cognitive or behavioral techniques to address symptoms and how patients responded clinically.
When psychotherapy is clearly documented, payer reviews become much easier to defend.
Identical or Copy-Pasted Notes for All Group Members
This error quietly destroys group therapy revenue and triggers audits faster than almost anything else.
Many practices use the same note template for all group members, changing only the patient name. From a payer’s perspective, this signals a lack of individualized treatment, which violates the requirements of psychotherapy.
Even though therapy is group-based, treatment is still individualized. Each patient has their own diagnosis, symptoms, and progress level.
Auditors compare notes across patients in the same session. When documentation is identical, they assume:
- Patients did not receive individualized care
- The provider did not clinically assess each participant
- The service may not qualify as psychotherapy
This often leads to the recoupment of multiple claims in a single session, not just in a single session.
Each patient’s note must stand on its own.
Documentation should reflect:
- How the patient participated
- What symptoms were addressed
- How the patient responded
- Any progress or barriers noted
The group topic can be similar, but patient response should never be identical. Even minor clinical differences protect against audit risk.
Training clinicians in individualized group documentation is one of the highest-ROI compliance steps a practice can take.
Missing or Invalid Diagnosis for Group Therapy Participants
Every patient billed under CPT 90853 must have a covered mental health diagnosis. This seems obvious, yet it is frequently missed.
Some practices enroll patients in group therapy before a diagnosis is fully documented. Others use vague or outdated diagnosis codes that no longer support medical necessity.
In payer audits, diagnosis validation is often the first checkpoint.
If a diagnosis:
- Is missing
- Does not justify group psychotherapy
- This is inconsistent with the treatment plan
The claim is denied, even if the therapy session itself was appropriate.
Payers do not reimburse group therapy for general stress, life coaching, or wellness goals without a covered diagnosis.
Before group enrollment:
- Confirm a documented DSM-aligned diagnosis
- Ensure it supports group psychotherapy
- Align the diagnosis with treatment goals
Diagnoses should be reviewed periodically, especially for long-term group therapy. Updated diagnoses strengthen medical necessity and protect reimbursement.
No Authorization or Incorrect Authorization for CPT 90853
Authorization errors are among the most preventable sources of revenue loss in group psychotherapy.
Many plans require prior authorization for group therapy, even when individual therapy does not. Others approve group therapy for a limited number of sessions.
A common mistake is assuming authorization for individual therapy automatically covers group therapy. In most cases, it does not.
Payers match claims against authorization data. If CPT 90853 is not explicitly approved, the claim is automatically denied, regardless of documentation quality.
Using authorization for the wrong CPT code is treated the same as having no authorization.
Authorization tracking must be CPT-specific, not patient-specific.
Best practices include:
- Obtaining separate authorization for 90853
- Tracking group sessions independently
- Monitoring visit limits closely
Billing teams should never assume coverage. Insurance Verification before the first group session prevents weeks of unpaid work.
Provider Not Credentialed or Approved to Bill Group Therapy
Not every licensed provider can bill CPT 90853 under every payer.
Some insurance plans restrict group psychotherapy billing to specific provider types or require additional credentialing. Others limit supervision arrangements for trainees or interns.
Practices often assume credentialing for individual therapy automatically applies to group therapy. That assumption is risky.
If the rendering provider:
- Is not credentialed for group therapy
- Is outside their scope of practice
- Does not meet payer supervision rules
The claim is denied as non-covered, even if the treatment was delivered correctly.
Before launching group therapy:
- Confirm provider credentialing with each payer
- Review the scope of practice limitations
- Verify supervision requirements for trainees
Credentialing errors can affect dozens of claims at once. Fixing them early protects both revenue and compliance.
Final Expert Takeaway
CPT code 90853 is one of the most efficient tools in behavioral health, but only when billed correctly.
Group therapy demands discipline. Documentation must be individualized. Authorization must be accurate. Medical necessity must be clear.
Practices that respect payer logic turn group psychotherapy into a stable revenue stream. Practices that treat it casually invite denials and audits.
When CPT 90853 is handled with precision, it supports better outcomes, stronger compliance, and sustainable growth for behavioral health providers across the USA.
Stop Losing Revenue on Group Therapy Billing
CPT 90853 billing errors quietly reduce reimbursement and increase audit risk for behavioral health practices. A2Z Medical Billing Company, based in New York, specializes in behavioral health billing and coding services, including group psychotherapy, authorization management, and denial prevention.
Our team ensures CPT 90853 is billed correctly, documentation meets payer standards, and reimbursements are maximized—without compliance risk.
👉 Partner with A2Z Medical Billing for reliable behavioral health billing and coding support across the USA.