Applied Behavior Analysis billing is not simple. It looks straightforward on paper, but in real life, it is one of the most denial-prone areas in behavioral health. ABA services involve time-based codes, multiple provider roles, strict authorizations, and payer-specific rules that change often. One small mistake can delay payment for weeks or wipe out margins entirely.
This guide is written from an RCM and medical billing expert’s point of view. It explains how ABA billing actually works in the U.S. healthcare system. We will cover CPT codes, ICD-10 linkage, authorizations, documentation, common denials, and payer rules. The goal is to help ABA providers bill correctly, stay compliant, and protect revenue.
ABA Services in the U.S. Healthcare System
ABA therapy is most commonly used for individuals with autism spectrum disorder and other developmental conditions. Services are typically delivered in clinics, homes, schools, or community settings. Unlike general psychotherapy, ABA services are highly structured and data-driven.
From a billing standpoint, ABA is classified as behavioral health, but many payers treat it as a specialized benefit. Coverage rules differ between Medicaid, commercial plans, and employer-funded policies. Medicare generally does not cover ABA services, which makes payer knowledge critical.
According to industry data, over 70% of ABA claim denials are related to authorization issues, time-based errors, or documentation gaps. Understanding the billing process is the only way to reduce that risk.
Common ICD-10 Diagnoses Used in ABA Billing
ABA billing almost always starts with a diagnosis. Without the correct ICD-10 code, no ABA service is payable.
The most common diagnosis is F84.0 – Autism spectrum disorder. Some payers also allow related developmental diagnoses, but autism remains the primary driver of coverage.
Other diagnoses sometimes used include:
- F84.9 Pervasive developmental disorder, unspecified
- F80.9 Developmental disorder of speech and language, unspecified
- F90.0 ADHD, predominantly inattentive type
However, many payers restrict ABA coverage strictly to autism diagnoses. Billing ABA under unsupported ICD-10 codes is a fast path to denial.
Documentation must clearly support the diagnosis. Most payers require a formal diagnostic evaluation completed by a qualified professional and updated periodically.
ABA CPT Codes
ABA CPT codes fall under the Category I behavior analysis codes. These are time-based and role-specific, which makes them different from standard therapy codes.
Assessment Codes
ABA billing often begins with assessment services. These codes support initial evaluation and treatment planning.
- 97151 is used for behavior identification assessment performed by a qualified healthcare professional. A BCBA typically bills this code, which is not time-based like treatment codes.
- 97152 may be used for supporting assessment services performed by a technician under supervision, depending on payer rules.
Assessment codes often require prior authorization and detailed reports. Many payers limit how frequently these services can be billed, usually once per year or per treatment cycle.
Treatment Codes
Treatment is where most ABA revenue comes from, and where most errors occur.
- 97153 is used for adaptive behavior treatment delivered by a technician under supervision. This is a time-based code, billed in 15-minute increments.
- 97155 is used when the supervising clinician, usually a BCBA, is actively involved in protocol modification or direct treatment.
- 97156 is billed for family adaptive behavior treatment guidance. This code supports caregiver training and education.
- 97158 is used for group adaptive behavior treatment.
Each of these codes has specific supervision, documentation, and time requirements. Mixing them incorrectly leads to denials or downcoding.
Time-Based Billing Rules in ABA
Time-based billing is the backbone of ABA reimbursement. Most ABA CPT codes are billed in 15-minute units, and payers are strict about accuracy.
Billing more units than documented is a common audit trigger. Billing fewer units than provided results in lost revenue.
Payers expect:
- Start and stop times
- Total minutes per session
- Units calculated correctly
- Clear separation of technician time and supervisor time
According to payer audit data, time calculation errors account for nearly 25% of ABA recoupments.
Authorizations in ABA Billing
ABA services almost always require prior authorization. This includes assessments, treatment hours, and sometimes caregiver training.
Authorization requests are driven by:
- ICD-10 diagnosis
- Severity of symptoms
- Functional deficits
- Treatment goals
- Requested hours per week
Submitting vague treatment plans or unsupported diagnoses leads to partial approvals or denials. Many payers approve fewer hours than requested, which directly affects revenue.
Experienced billing teams track:
- Authorized hours
- Date ranges
- CPT code limits
- Provider type restrictions
Billing outside authorization is one of the most expensive mistakes in ABA practices.
Documentation Requirements for ABA Claims
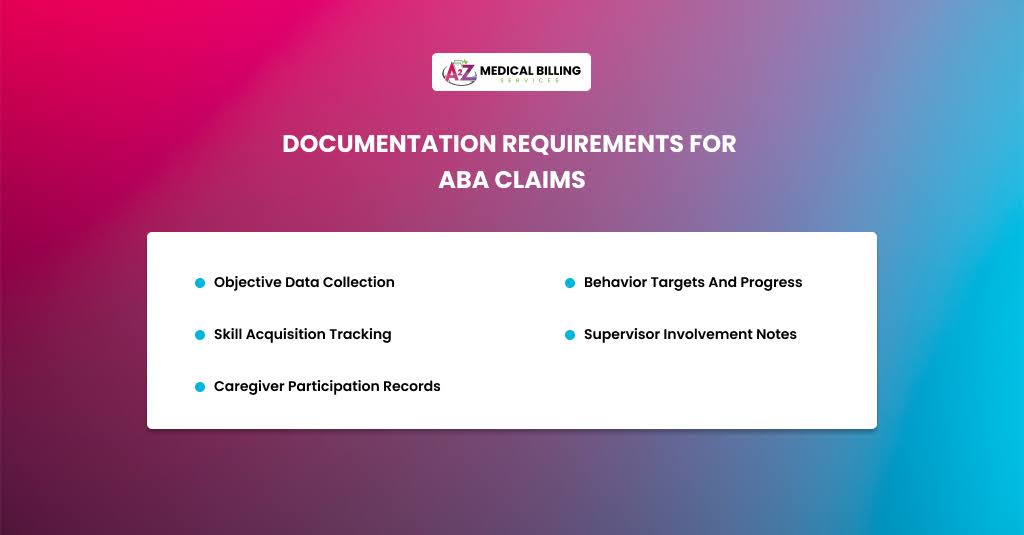
ABA documentation must be detailed, consistent, and defensible. Payers review notes closely, especially during audits.
Strong documentation includes:
- Objective data collection
- Behavior targets and progress
- Skill acquisition tracking
- Supervisor involvement notes
- Caregiver participation records
Notes should clearly support the CPT code billed. For example, billing 97155 requires proof that the supervisor was actively involved, not just present.
If it is not documented, it does not exist in the payer’s eyes.
Linking CPT Codes With ICD-10 for Medical Necessity
Medical necessity is the core of ABA billing. Payers look at whether the diagnosis justifies the intensity of services.
High weekly hours must be supported by:
- Severe functional impairment
- Safety concerns
- Limited adaptive skills
Using F84.0 alone is not enough. Documentation must explain how autism impacts daily functioning and why ABA is necessary.
Claims with weak medical-necessity language are often denied during utilization review or a post-payment audit.
Payer-Specific ABA Billing Considerations
Medicaid
Medicaid is the largest payer for ABA services. Coverage rules vary by state, but documentation and authorization requirements are strict.
Many states require:
- Annual re-evaluations
- Progress reports
- Specific provider credentials
Commercial Insurance
Commercial payers follow medical policies that define hour limits, age restrictions, and approved CPT codes.
Some plans cap annual hours or require periodic reauthorization every few months.
Self-Funded Plans
Employer-funded plans may follow different rules and require direct communication with plan administrators.
Knowing the payer type is critical before billing ABA services.
Common ABA Billing Denials and How to Avoid Them
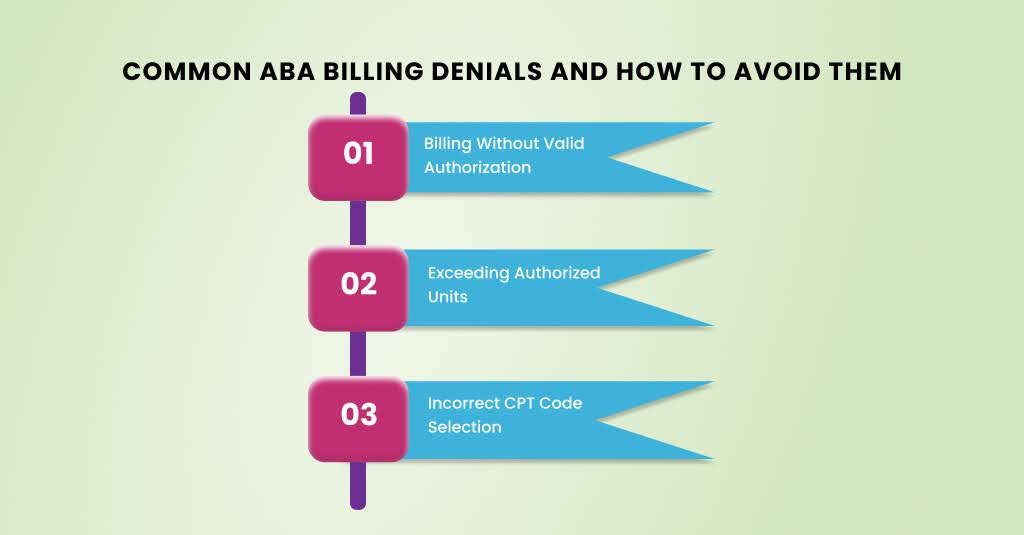
ABA billing denials follow patterns. After years of working with ABA providers, the same issues keep popping up. These denials are rarely random. Most of them stem from small workflow gaps that quietly accumulate until payers stop paying.
Understanding why ABA claims are denied is the first step. Fixing the process behind those denials is what protects long-term revenue. Below is a deep, real-world breakdown of the most common ABA billing denials and how experienced billing teams prevent them.
Billing Without Valid Authorization
This is the number one denial reason in ABA billing.
Most payers require prior authorization for assessments, treatment hours, and caregiver training. If services are provided outside the authorized date range, exceed the approved hours, or use CPT codes not listed on the authorization, the claim is automatically denied.
What makes this worse is that many ABA sessions are delivered daily. By the time the denial is noticed, weeks of services may already be unpaid.
Avoiding it starts with strong tracking. Every ABA provider needs a live authorization log. It should include CPT codes, approved units, start and end dates, and provider type. Billing teams should review authorizations weekly, not monthly. Waiting until a claim is denied is already too late.
Exceeding Authorized Units
Even when an authorization exists, claims are still denied when billed units exceed the approved amount.
This often happens because clinical scheduling and billing are not aligned. Technicians may deliver more hours per treatment plan, while billing is limited by payer approval.
Payers do not pay for “medically appropriate” services if they were not authorized. They only pay for what they approved.
To avoid this, ABA providers must connect scheduling, clinical teams, and billing. Real-time unit tracking prevents overages. Many successful practices automatically stop sessions when units run low, unless a new authorization is in place.
This one fix alone can save thousands per month in lost revenue.
Incorrect CPT Code Selection
ABA CPT codes look similar, but payers treat them very differently.
For example, billing 97155 requires active protocol modification by a supervising clinician. Simply observing or checking notes does not qualify. When documentation does not support the CPT code billed, payers deny or downcode the claim.
Another common issue is billing 97153 and 97155 incorrectly during the same time period. Overlapping time or unclear role separation raises red flags during audits.
Avoiding this denial requires ongoing provider education. Clinicians and technicians must understand which activities match each CPT code. Billing teams should review notes regularly to confirm that the code matches the service provided.
According to payer audit reports, CPT mismatches account for nearly 20% of ABA recoupments.
Time-Based Billing Errors
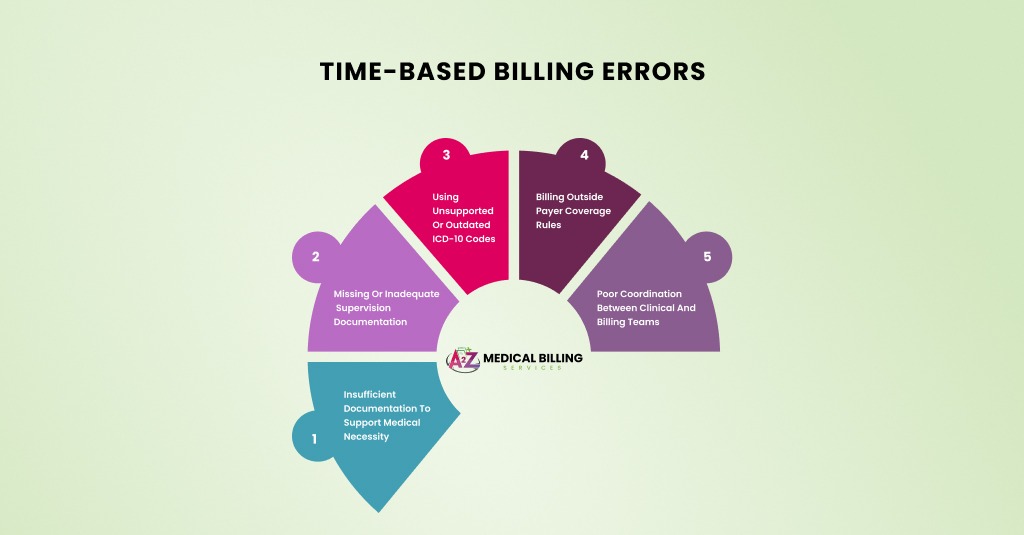
ABA services are time-driven. That makes time documentation a major risk area.
Common time-related denials include:
- Missing start and stop times
- Units that do not match the documented minutes
- Rounded time without justification
- Overlapping sessions billed separately
Payers expect precise math. Fifteen-minute units must be calculated correctly every time. Billing extra units without supporting minutes is one of the fastest ways to trigger audits.
To avoid this, ABA practices should standardize the timing of documentation. Notes should clearly show session length, breaks, and total billable time. Billing teams should spot-check units before claims go out.
Even small-time errors, when repeated, can lead to large takeaways.
Insufficient Documentation to Support Medical Necessity
Medical necessity denials are among the hardest to overturn.
Payers review whether the diagnosis, severity, and functional impairment justify the number of hours billed. Simply stating “autism” is not enough. Documentation must explain how symptoms impact daily functioning and why ABA is required at the current intensity.
High weekly hours without a clear justification almost always trigger review. Notes that lack objective data, progress tracking, or behavior descriptions weaken the claim.
Avoiding this denial requires stronger clinical documentation. Notes should show measurable goals, progress or lack of progress, and ongoing need for treatment. Supervisory notes are essential for higher-level codes.
Practices that use structured documentation templates report far fewer medical-necessity denials.
Missing or Inadequate Supervision Documentation
Supervision rules are strict in ABA billing.
When billing technician services, payers expect clear evidence of qualified supervision. When billing supervisory codes, they expect proof of active involvement.
Denials happen when notes do not clearly show:
- Who supervised the session?
- What supervisory activities occurred
- How treatment protocols were modified
Without this detail, payers assume supervision did not occur.
The fix is simple but requires discipline. Supervisors should document their role in plain language. Billing teams should flag notes that lack sufficient supervisory detail before submitting claims.
Using Unsupported or Outdated ICD-10 Codes
ABA billing is diagnosis-driven. Most payers require F84.0 Autism spectrum disorder to approve services. Using unsupported ICD-10 codes leads to automatic denial.
Another issue is failing to update diagnoses over time. Some payers require periodic re-evaluations and updated diagnostic documentation. Billing under an old diagnosis without current support raises audit risk.
Avoid this by tracking diagnosis review dates and payer-specific requirements. Keep diagnostic evaluations current and aligned with claims.
Billing Outside Payer Coverage Rules
Every payer has its own medical policy for ABA services. These policies define:
- Age limits
- Annual hour caps
- Covered CPT codes
- Required provider credentials
Billing outside these rules leads to denials, even when services were provided correctly.
Experienced billing teams keep payer policies up to date and accessible. They do not rely on assumptions or old approvals. Reviewing policies annually helps avoid unnecessary denials.
Poor Coordination Between Clinical and Billing Teams
Many ABA denials are not technical. They are communication failures.
Clinical teams deliver services. Billing teams submit claims. When they do not talk, errors happen. Authorizations expire. Units exceed limits. Documentation misses key details.
Practices that hold regular clinical-billing meetings see fewer denials and faster payments. Shared responsibility improves outcomes on both sides.
Final Thoughts
ABA billing is detailed, regulated, and unforgiving. But when done correctly, it supports stable and predictable revenue. The key is understanding how diagnoses, CPT codes, authorizations, and documentation work together.
ABA providers who treat billing as part of care delivery, not just paperwork, see fewer denials and stronger financial outcomes. Clean ABA billing protects your practice and ensures services continue without disruption for the families who depend on them.



