Benign Prostatic Hyperplasia (BPH) — also known as prostate gland enlargement — is one of the most common urological conditions in men over 50. While the clinical management is straightforward, billing and coding for BPH often aren’t.
The coding depends on whether the patient has symptoms, complications, or related urinary issues like obstruction or retention. Missing those distinctions can mean denied or underpaid claims.
In this guide, we’ll break down everything you need to know — from ICD-10 codes and documentation requirements to CPT pairings, payer rules, and revenue optimization.
Understanding Benign Prostatic Hyperplasia (BPH)
Before you code it, it’s worth understanding what BPH actually means in clinical and billing terms.
BPH is a non-cancerous enlargement of the prostate gland that commonly causes lower urinary tract symptoms (LUTS), such as:
- Frequent urination, especially at night
- Difficulty starting urination
- Weak urine stream or dribbling
- Incomplete bladder emptying
From a billing standpoint, these symptoms matter because they affect which ICD-10 code you’ll use and whether you can bill for additional services (like urinalysis, cystoscopy, or ultrasound).
ICD-10 Codes for BPH
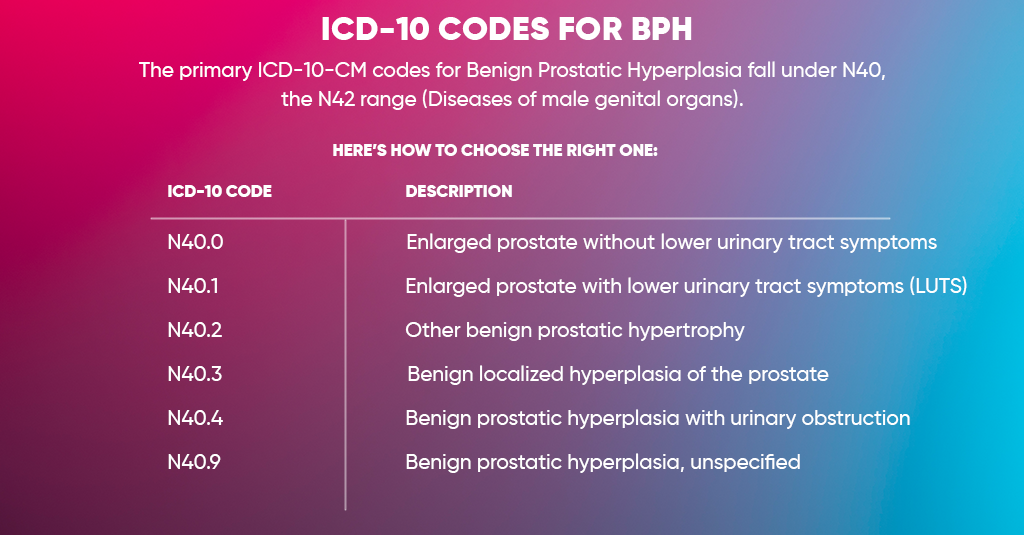
The primary ICD-10-CM codes for Benign Prostatic Hyperplasia fall under N40, the N42 range (Diseases of male genital organs).
Here’s how to choose the right one:
| ICD-10 Code | Description |
| N40.0 | Enlarged prostate without lower urinary tract symptoms |
| N40.1 | Enlarged prostate with lower urinary tract symptoms (LUTS) |
| N40.2 | Other benign prostatic hypertrophy |
| N40.3 | Benign localized hyperplasia of the prostate |
| N40.4 | Benign prostatic hyperplasia with urinary obstruction |
| N40.9 | Benign prostatic hyperplasia, unspecified |
Common Associated Conditions and Secondary Codes
BPH often coexists with urinary symptoms that need additional coding to support medical necessity.
Here are some secondary or supporting ICD-10 codes commonly linked with BPH claims:
| Condition | ICD-10 Code |
| Urinary retention | R33.9 |
| Hematuria (blood in urine) | R31.9 |
| Dysuria (painful urination) | R30.0 |
| Urgency of urination | R39.15 |
| Nocturia | R35.1 |
| Urinary frequency | R35.0 |
| Incomplete bladder emptying | R39.14 |
Including these secondary codes helps payers understand the severity and medical necessity for diagnostic or procedural interventions.
CPT Codes Commonly Billed with BPH
BPH-related visits often include evaluations, diagnostic tests, and procedures.
Below are frequently used CPT codes that may appear alongside BPH diagnoses:
| Procedure / Service | CPT Code |
| Office or outpatient E/M visit | 99202–99215 |
| Prostate ultrasound (transrectal) | 76872 |
| Uroflowmetry | 51741 |
| Post-void residual measurement | 51798 |
| Cystourethroscopy | 52000 |
| Urodynamic studies | 51728–51729 |
| Prostate biopsy (needle) | 55700 |
| Laser prostatectomy | 52648 |
| TURP (Transurethral Resection of Prostate) | 52601 |
Billing and Coding Guidelines for Benign Prostatic Hyperplasia (BPH)
Billing for Benign Prostatic Hyperplasia (BPH) requires more than just listing N40.0 or N40.1 on the claim. Payers look closely at clinical documentation, coding accuracy, and medical necessity before approving payment — especially since many BPH treatments involve diagnostic tests, imaging, or surgical procedures that can be costly.
To get your claims approved smoothly and avoid denials, your coding and documentation need to tell a complete clinical story — from the patient’s symptoms to the rationale for each test or treatment. Here’s how to do it right.
Document All Symptoms Clearly
Every clean BPH claim begins with detailed documentation. Don’t just write “BPH” in the note — describe the patient’s actual urinary symptoms. Include common findings such as:
- Increased frequency or urgency
- Nocturia (waking up multiple times at night to urinate)
- Hesitancy, weak stream, or incomplete emptying
- Urinary retention or post-void dribbling
These symptoms help establish medical necessity for diagnostic tests and procedures. Payers expect to see evidence that the patient’s symptoms justify evaluation or intervention — not just a “routine check.”
Link the Correct Diagnosis Codes
Accuracy in diagnosis coding is critical for reimbursement. The ICD-10-CM codes for BPH differentiate between cases with and without lower urinary tract symptoms (LUTS):
- N40.0 – Benign prostatic hyperplasia without lower urinary tract symptoms
- N40.1 – Benign prostatic hyperplasia with lower urinary tract symptoms
- N40.2–N40.3 (for obstruction or other complications, if documented)
- N40.9 – Benign prostatic hyperplasia, unspecified (use only when documentation is unclear)
When you pair these with CPT codes, make sure the procedure matches the diagnosis. For example, N40.1 is appropriate for flow studies, cystoscopy, or medication management related to LUTS, while N40.0 might support basic evaluations or screenings.
Inconsistent pairing (like billing N40.0 for a patient treated for urinary obstruction) can result in denials for lack of medical necessity.
Use Modifiers When Needed
Modifiers play a key role in BPH billing, mainly when multiple services occur during the same encounter.
For instance, if a provider performs an evaluation and management (E/M) service along with a diagnostic test like a uroflowmetry or ultrasound, you’ll need to append modifier -25 to the E/M code.
This tells the payer that the E/M visit was significant and separately identifiable from the procedure, not just part of the pre-procedure work.
Similarly, modifier -59 may be required when multiple urologic procedures are performed on the same day but are clinically distinct (e.g., cystoscopy and flow rate study).
Correct modifier usage prevents claims from being “bundled” or denied as duplicates.
Check Payer LCD/NCD Policies
Not all BPH-related services are covered equally. Medicare and other payers often publish Local Coverage Determinations (LCDs) or National Coverage Determinations (NCDs) outlining which tests and procedures they consider medically necessary.
For example, some LCDs specify how often a uroflowmetry test (CPT 51741) or post-void residual measurement (CPT 51798) can be billed per patient per year.
Before submitting claims, verify:
- Whether prior authorization is required for procedures like TURP (CPT 52601) or laser prostatectomy (CPT 52648).
- If there are documentation requirements, such as failed medication therapy, before surgery is approved, then [complete the sentence].
Ignoring payer policies is one of the fastest ways to trigger denials or post-payment reviews.
Include Test Results in Documentation
Supporting evidence matters just as much as the diagnosis code. Whenever you bill for BPH-related testing or procedures, attach or reference the clinical results that justify them.
Examples include:
- Post-void residual (PVR) measurements showing incomplete bladder emptying
- Uroflowmetry results indicate a weak stream
- Cystoscopy or ultrasound findings showing prostate enlargement or obstruction
These details strengthen your claim’s medical necessity and protect against audits. Payers expect to see objective proof that diagnostic procedures weren’t performed “routinely” but were needed based on patient symptoms.
Avoid Overuse of Unspecified Codes (N40.9)
Using N40.9 (Benign prostatic hyperplasia, unspecified) might seem convenient, but it signals incomplete documentation. Frequent use of unspecified codes can lead to payment delays or even payer audits.
Providers should always document whether the patient has lower urinary tract symptoms (LUTS) or other complications. If the chart lacks those details, coders should query the provider before submitting.
The difference between N40.0 and N40.1 isn’t just a coding detail — it directly affects coverage for many urologic procedures.
Ensure Consistency Across Documentation, Coding, and Billing
A successful BPH claim should tell one clear, consistent story.
The provider’s note, ICD-10 code, and CPT procedure must all align logically. For instance, if your documentation describes “BPH with nocturia and weak stream,” your diagnosis should be N40.1, not N40.0.
A mismatch between documentation and billing can easily trigger payer reviews or recoupments. Consistency is what keeps your revenue cycle compliant and audit-proof.
Keep Up with Annual Coding Updates
ICD-10 and CPT codes are updated yearly, and urology is one of the specialties most affected by these changes. Always stay current on:
- New procedural codes for minimally invasive BPH treatments (like UroLift or Rezūm) are available.
- Revised LCD policies or frequency limitations.
- Modifier and bundling edits (especially for E/M with diagnostics).
Ongoing staff training and annual code reviews can save thousands in potential rework or lost reimbursement.
How to Avoid Common Billing Errors
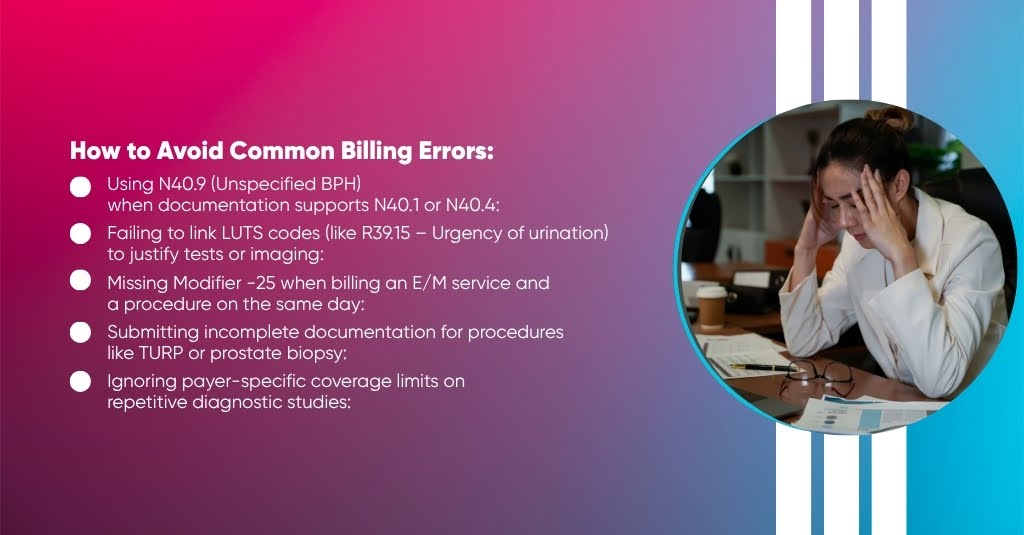
Even the best urology practices lose thousands each year over small, avoidable billing mistakes. BPH claims are especially vulnerable because they involve detailed coding rules, frequent procedures, and payer-specific coverage policies. The good news? Most of these errors can be fixed with sharper documentation and a few habit changes.
Here’s what to watch for when billing for Benign Prostatic Hyperplasia (BPH):
Using N40.9 (Unspecified BPH) when documentation supports N40.1 or N40.4:
Unspecified codes might seem convenient, but they raise red flags for auditors. Always code to the highest level of specificity. If your notes mention symptoms like frequency or nocturia, go with N40.1 (BPH with LUTS) instead of N40.9.
Failing to link LUTS codes (like R39.15 – Urgency of urination) to justify tests or imaging:
If you’re billing for diagnostic tests such as uroflowmetry, ultrasound, or cystoscopy, make sure to link appropriate symptom codes. They tell payers why the test was medically necessary, not just that it was performed.
Missing Modifier -25 when billing an E/M service and a procedure on the same day:
Forgetting this one modifier can cause instant denials. Always append modifier -25 when a significant, separately identifiable E/M service is done along with a diagnostic procedure (like uroflowmetry or PVR measurement). It distinguishes the visit as more than routine pre-procedure work.
Submitting incomplete documentation for procedures like TURP or prostate biopsy:
Payers require clinical justification for invasive procedures. Always include prior treatment history (like failed medication), test results, and symptom progression in your notes. Missing these details can make even a legitimate claim look unjustified.
Ignoring payer-specific coverage limits on repetitive diagnostic studies:
Medicare and commercial payers often limit how often certain BPH-related studies—like uroflowmetry or bladder scans—can be billed per year. Review Local Coverage Determinations (LCDs) before submitting claims to avoid frequency-based denials.
Conclusion
ICD-10 coding for Benign Prostatic Hyperplasia (BPH) isn’t just about accuracy — it’s about clarity, compliance, and cash flow. Every single detail in your documentation — from how you describe LUTS symptoms (like nocturia, urgency, or weak stream) to the diagnostic findings that confirm enlargement — directly impacts whether your claim gets paid quickly or stuck in denial limbo.
Precise documentation gives coders the confidence to assign the correct ICD-10 and CPT combinations. It also tells payers that your medical decisions are clinically justified and supported by evidence — not guesswork. When your claim reflects the accurate picture of the patient’s condition, insurers have little room to challenge it.
Inconsistent charting (like using “BPH, unspecified” too often) might not seem like a big deal. Still, it signals incomplete care documentation to payers — and that’s precisely what triggers audits, recoupments, and delayed payments. The difference between N40.0 (BPH without LUTS) and N40.1 (BPH with LUTS) can literally mean hundreds of dollars per encounter and far smoother reimbursement.
Let’s Turn Your BPH Billing Challenges Into Steady, Predictable Revenue
If your claims keep getting delayed or underpaid, it’s time to simplify the process.
At A2Z Medical Billing, we handle your BPH coding and billing from start to finish — eligibility checks, clean code pairing, claim submission, denial management, and payer follow-ups.



