Type 2 diabetes coding goes far beyond assigning a single diagnosis code. ICD-10-CM category E11 is designed to capture not only the presence of diabetes but also its full clinical impact complications, disease control, and long-term management. From hyperglycemia and kidney disease to neuropathy, retinopathy, vascular issues, and medication use, each detail matters. Accurate E11.x coding directly affects reimbursement, risk adjustment, quality reporting, and compliance. This guide breaks down every major E11 subcategory and common coding scenario so coders can confidently translate provider documentation into precise, defensible claims that reflect actual disease severity.
What is Type 2 Diabetes Mellitus
Type 2 diabetes mellitus (T2DM) is a chronic metabolic disorder characterized by insulin resistance and impaired glucose regulation. In ICD-10-CM, T2DM is coded under E11, which includes all patients diagnosed with Type 2 diabetes, regardless of whether they are managed with diet, oral medications, insulin, or a combination.
Most patients have complications or comorbid conditions that must be reported with E11.x subcodes, as the base code E11 alone is rarely sufficient. Accurate coding is critical for compliance, reimbursement, risk adjustment, and reflection of disease severity.
Coders should verify three key elements in provider documentation before assigning a code:
Presence of complications: Kidney disease, neuropathy, retinopathy, foot ulcers, or vascular issues.
Diabetes status: Controlled, poorly controlled, hyperglycemic, or hypoglycemic.
Long-term therapy: Insulin (Z79.4) or oral antidiabetic medications (Z79.84).
E11.65 – Type 2 Diabetes Mellitus With Hyperglycemia
Definition: E11.65 is used for T2DM patients experiencing elevated blood glucose or poor glycemic control. This includes any description of “uncontrolled” or “hyperglycemic” diabetes.
Documentation examples:
- “Patient has persistent hyperglycemia despite oral therapy.”
- “Type 2 diabetes poorly controlled on metformin.”
- “Blood glucose readings elevated above target range.”
Key points:
- E11.65 is used regardless of the presence of insulin therapy.
- Avoid using E11.65 if the patient is stable or at target glucose levels; in those cases, E11.9 is appropriate.
- Long-term medication use may require secondary Z-codes.
Coding Tip: Even short-term hyperglycemia should be documented clearly. If a steroid or illness temporarily elevates glucose, clarify whether the episode is linked to diabetes for proper coding.
E11.2 Series – Diabetes With Kidney Complications
Kidney complications are among the most common and serious issues in T2DM. The E11.2 series includes nephropathy, chronic kidney disease (CKD), and other kidney complications.
E11.21 – Diabetic Nephropathy
Assign this when documentation confirms kidney damage directly related to diabetes.
Examples:
- “Diabetic nephropathy with albuminuria”
- “Renal impairment secondary to diabetes”
Note: CKD stage is not required unless specified. If CKD stage is documented, add N18.x to indicate stage.
E11.22 – Diabetes With CKD
Used when the patient has chronic kidney disease attributed to diabetes. Two codes are required:
- E11.22 – Type 2 diabetes with CKD
- N18.x – CKD stage (N18.1–N18.5 for stages 1–5, N18.6 for ESRD, N18.9 for unspecified)
Example: “Type 2 diabetes with CKD stage 3” → E11.22 + N18.3
Important: For ESRD, also check for dialysis codes.
E11.29 – Other Kidney Complications
For diabetes-related kidney involvement not classified as nephropathy or CKD stage.
Examples: Early renal changes, diabetic renal disorder unspecified.
Coding Tip: Always clarify whether the complication is diabetes-related if the note is ambiguous.
E11.3 Series – Diabetes With Ophthalmic Complications
Diabetic eye complications, especially retinopathy, are critical for accurate coding.
E11.31 – Unspecified Diabetic Retinopathy
Use when retinopathy is documented, but the type, severity, or laterality is unclear.
Documentation examples:
- “Diabetic retinopathy.”
- “Retinopathy due to diabetes.”
- “Changes consistent with diabetic eye disease.”
E11.32–E11.39 – Specific Retinopathy Codes
If documentation specifies:
- Severity (mild, moderate, severe)
- Type (NPDR, PDR)
- Macular edema presence or absence
- Laterality (right, left, bilateral)
Example: “Moderate NPDR with macular edema, right eye” → assign the corresponding E11.3x code.
Tip: Always capture severity, edema, and laterality to prevent undercoding.
E11.4 Series – Diabetes With Neurological Complications
Neuropathy is the most frequent neurological complication of diabetes.
E11.40 – Unspecified Diabetic Neuropathy
Use when documentation states “diabetic neuropathy” without specifying the type.
E11.41 – Diabetic Mononeuropathy
Applies to single nerve involvement, such as:
- Median nerve palsy
- Ulnar neuropathy
- Cranial nerve involvement
E11.42 – Diabetic Polyneuropathy
Most common form; includes bilateral foot neuropathy or systemic peripheral neuropathy.
E11.43 – Diabetic Autonomic Neuropathy
For autonomic involvement, such as:
- Gastroparesis
- Orthostatic hypotension
- Diabetic bladder dysfunction
Tip: Document type clearly; coding requires precision between mononeuropathy, polyneuropathy, and autonomic neuropathy.
E11.5 Series – Diabetes With Circulatory Complications
Vascular complications impact T2DM morbidity and billing.
E11.51 – Peripheral Angiopathy
Documented PAD or PVD due to diabetes. Combine with I73.x if needed.
Example: “Diabetic patient with lower extremity PAD” → E11.51 + I73.9
E11.52 – Diabetes With Gangrene
Use when gangrene is linked to diabetes, and specify the location using I96 or L97.x for ulcers.
Example: “Gangrene of right forefoot due to diabetes” → E11.52 + I96 + L97.x
E11.59 – Other Circulatory Complications
Catch-all code for vascular complications not otherwise specified, e.g., early microangiopathy.
Coding Tip: Laterality and ulcer presence must be documented.
E11.6 Series – Skin & Ulcer Complications
Skin and soft tissue complications include foot ulcers, non-foot ulcers, infections, and other skin conditions.
E11.621 – Diabetes With Foot Ulcer
Requires combination with L97.x to specify site, laterality, depth, and severity.
Example: “Left heel ulcer with bone involvement” → E11.621 + L97.423
E11.622 – Diabetes With Other Skin Ulcers
For ulcers not on the foot, e.g., a diabetic calf ulcer.
E11.628 – Other Skin Complications
Includes:
- Diabetic dermatitis
- Skin infections linked to diabetes
- Diabetic bullae
- Necrobiosis lipoidica
E11.69 – Other Specified Complications
Used when complications are clear but do not fit into kidney, eye, neurological, circulatory, or skin categories. Examples:
- Gastrointestinal complications
- Diabetic arthropathy
Coding Tip: Avoid using E11.69 as a fallback; always ensure the complication is clearly documented.
E11.8 – Diabetes With Unspecified Complications
E11.8 is used when a complication exists but cannot be specifically identified.
Documentation examples:
- “Diabetes with complications.”
- “Systemic diabetic involvement.”
Tip: If the complication is identifiable, assign the appropriate E11.x code rather than E11.8.
E11.9 – Type 2 Diabetes Without Complications (Extended Clarification)
E11.9 is for patients with no documented complications or who are stable/well-controlled.
Additional Z-codes may apply:
· Z79.4 – Long-term insulin use
· Z79.84 – Long-term oral antidiabetic therapy
· Z71.3 – Dietary counseling (if applicable)
Key Distinction: E11.8 vs E11.9
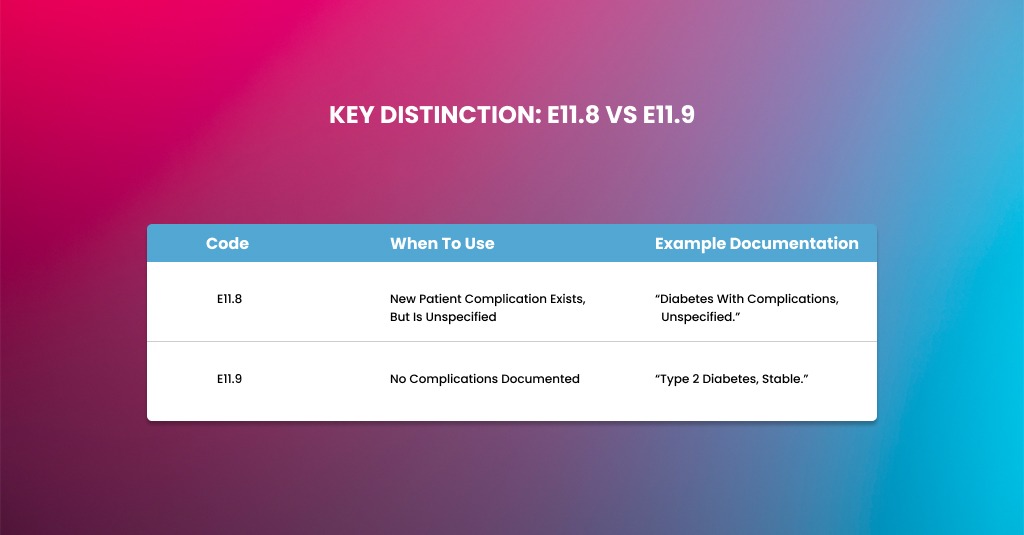
| Code | When to Use | Example Documentation |
| E11.8 | Complication exists, but is unspecified | “Diabetes with complications, unspecified.” |
| E11.9 | No complications documented | “Type 2 diabetes, stable.” |
ICD-10 Combination Coding for Type 2 Diabetes
Combination coding ensures the diabetes code reflects complications and management.
Common combinations include:
- E11.22 + N18.x – Diabetes with CKD, specify stage
- E11.621 + L97.x – Diabetes with foot ulcer
- E11.52 + I96 (+ L97.x) – Diabetes with gangrene
- E11.51 + I73.x – Diabetes with PAD
- E11.3x + H54.x – Diabetes with vision loss
Tip: Always document severity, laterality, and secondary conditions.
Z79.4 & Z79.84 – Long-Term Medication Use With Diabetes
- Z79.4 – Long-term insulin use (assign only if chronic)
- Z79.84 – Long-term oral medications (metformin, SGLT2 inhibitors, etc.)
- Both can be assigned if the patient uses insulin and oral meds concurrently.
Necessary: Do not assign Z79.4 for Type 1 diabetes; insulin use is inherent to the disease.
Pediatric Coding for Type 2 Diabetes (E11 Series)
Children are coded as E11.x series as adults.
- No complications → E11.9
- Complications present → assign specific E11.x subcode (e.g., E11.65 for hyperglycemia, E11.21 for nephropathy)
- Long-term medication → Z79.4 or Z79.84
Prediabetes or isolated hyperglycemia should not be coded as E11:
- R73.03 – Prediabetes
- R73.9 – Hyperglycemia, unspecified
Note: Pediatric documentation often involves obesity, insulin resistance, or atypical presentations. Coders should ensure the type of diabetes is explicitly stated.
Billing & Coding Mistakes in Type 2 Diabetes and How to Avoid Them
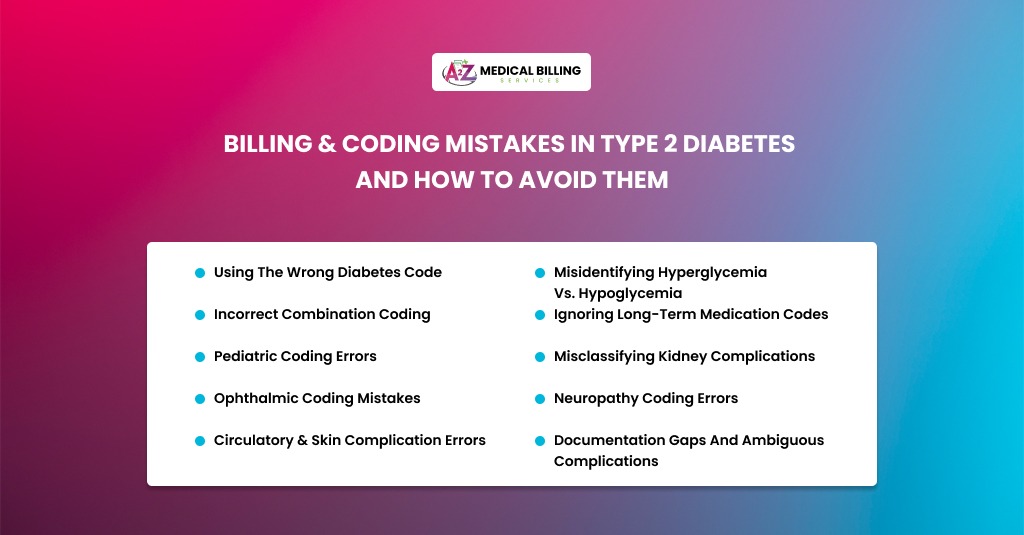
Using the Wrong Diabetes Code
Choosing the correct ICD-10 code for Type 2 diabetes is more than a formality—it directly impacts reimbursement, reporting, and clinical accuracy. A common mistake is defaulting to E11.9 (Type 2 diabetes without complications) without checking whether the patient has documented complications. Even subtle indications of neuropathy, kidney disease, retinopathy, or vascular issues require a more specific E11.x code to reflect the patient’s condition accurately. Always review the provider’s documentation for complications such as neuropathy, CKD, retinopathy, or vascular disease.
- Assign the most specific E11.x code based on the documented complication.
- Query the provider if complications are unclear or not explicitly linked to diabetes.
Misidentifying Hyperglycemia vs. Hypoglycemia
Confusing hyperglycemia with hypoglycemia is a frequent coding pitfall. Hyperglycemia involves elevated blood glucose, whereas hypoglycemia represents abnormally low levels, each requiring distinct codes. Mistakenly coding hyperglycemia for controlled diabetes, or using the wrong series for low blood sugar, can lead to claim denials and misrepresentation of the patient’s clinical status.
- Use E11.65 only when the provider documents poor control, elevated glucose readings, or hyperglycemic episodes.
- Use E11.64 series codes for documented hypoglycemia.
- Cross-check lab results, medication changes, and provider notes for confirmation.
Incorrect Combination Coding
Type 2 diabetes is often accompanied by secondary complications that need additional codes. A major error occurs when coders omit these secondary codes, resulting in incomplete or inaccurate claims. Whether it’s CKD, neuropathy, or foot ulcers, failing to combine the primary diabetes code with the appropriate secondary code can misrepresent disease severity and risk adjustment.
- Pair diabetes codes with appropriate secondary codes, e.g., E11.22 + N18.x for CKD stage, E11.621 + L97.x for foot ulcers.
- Always document the specific complication, stage, laterality, or site.
- Use combination codes even if only one complication is mentioned, provided it is confirmed as diabetes-related.
Ignoring Long-Term Medication Codes
Long-term use of insulin or oral antidiabetic medications must be reflected with Z79.4 or Z79.84. Coders sometimes overlook these codes, which can skew clinical documentation and risk adjustment data. Omitting these details can fail to capture ongoing management and affect both reimbursement and patient care tracking.
- Assign Z79.4 only for ongoing insulin therapy and Z79.84 for long-term oral hypoglycemics.
- Do not code Z79.x for short-term medication use.
- Document whether the therapy is chronic or intermittent.
Pediatric Coding Errors
Though Type 2 diabetes is less common in children, coding rules remain the same as for adults. Mistakes often arise when prediabetes or hyperglycemia is misclassified as Type 2 diabetes, leading to inaccurate claims. Pediatric coding requires careful attention to confirmed diagnoses, long-term medication use, and any documented complications.
- Use R73.03 for prediabetes and R73.9 for unspecified hyperglycemia.
- Only assign E11.x when the provider explicitly diagnoses Type 2 diabetes.
- Confirm long-term medication use and complications, even in pediatric patients.
Misclassifying Kidney Complications
Diabetes-related kidney issues are often miscoded because coders default to generic codes instead of specifying nephropathy, CKD, or other conditions. Misclassification affects not only reimbursement but also the accurate portrayal of disease progression. Capturing the exact type and stage of kidney involvement is critical for compliance and clinical accuracy.
- Verify whether the kidney complication is nephropathy, CKD, or another diabetes-related kidney condition.
- Include the CKD stage using N18.x codes when applicable.
- Query the provider if documentation is ambiguous regarding diabetic kidney involvement.
Ophthalmic Coding Mistakes
Diabetic retinopathy is a common complication that demands precise coding. Using unspecified codes when the provider has documented severity, laterality, or macular edema undermines coding accuracy and can affect both billing and patient risk stratification. An accurate E11.3x assignment ensures claims reflect the true clinical picture.
- Always capture the type of retinopathy, severity (mild, moderate, severe), macular edema presence, and laterality (right, left, bilateral).
- Assign the most specific E11.3x code supported by documentation.
- Query providers for missing details to ensure correct coding.
Neuropathy Coding Errors
Neurological complications, such as diabetic neuropathy, are frequently underreported or coded as unspecified. Failing to distinguish between mononeuropathy, polyneuropathy, or autonomic neuropathy can lead to incomplete documentation and improper reimbursement. Coders must carefully match the code to the documented type, severity, and affected nerve(s).
- Use E11.41 for diabetic mononeuropathy, E11.42 for polyneuropathy, and E11.43 for autonomic neuropathy.
- Confirm whether neuropathy is directly linked to diabetes.
- Include the site or nerve affected if documented.
Circulatory & Skin Complication Errors
Peripheral artery disease, gangrene, and diabetic skin ulcers are often miscoded or missing secondary codes, which leads to underreported severity. Accurate coding requires attention to ulcer type, laterality, depth, and associated complications. Missteps in this area can result in denied claims, audit issues, and misrepresentation of patient risk.
- Assign E11.51 + I73.x for PAD, E11.52 + I96 for gangrene, and E11.621 + L97.x for foot ulcers.
- Distinguish between pressure and non-pressure ulcers (use L89.x for pressure ulcers).
- Always document laterality, ulcer depth, and associated complications like neuropathy or PAD.
Documentation Gaps and Ambiguous Complications
Incomplete or unclear provider notes are a leading cause of billing and coding errors. Without clarification, coders risk undercoding, overcoding, or submitting inaccurate claims. Proper documentation review, queries for missing details, and inclusion of lab or imaging results are essential for coding accuracy, compliance, and risk adjustment.
- Query the provider for missing details or unclear complications.
- Ensure all complications are explicitly linked to Type 2 diabetes.
- Incorporate lab results, imaging, and clinical findings when coding complications.
Final Thoughts
ICD-10 coding for Type 2 diabetes demands specificity, documentation awareness, and consistent use of combination codes. Relying solely on E11.9 often understates the patient’s condition, while omitting secondary codes for complications or long-term therapy can distort clinical data and reimbursement. The key to accurate E11 coding is simple but disciplined: confirm the type of complication, link it clearly to diabetes, capture severity and laterality, apply required secondary and Z-codes, and query when documentation falls short. When done correctly, E11 coding does more than support clean claims—it tells the full clinical story of diabetes and ensures compliant, accurate, and optimized reporting across the care continuum.



