Incident-to billing may sound intimidating, but it’s actually a tool designed to maximize your practice’s efficiency and revenue. Think of it like giving your NP or PA a superpower—they can see patients and bill at the physician rate, but only if the rules are followed. This guide walks you through everything step by step.
What Is Incident-to Billing?
Incident-to billing is a way for your practice to bill Medicare—or certain private insurers—as if the physician personally performed a service, even when it was provided by a non-physician provider like a nurse practitioner (NP), physician assistant (PA), or other qualified clinical staff.
Why does this matter? Well, here’s the financial angle: non-physician providers usually get reimbursed at a lower rate—typically around 85% of the physician’s rate. Incident-to lets your practice capture 100% of the physician’s rate, legally. That difference can add up fast. Imagine an NP visit reimbursed at $100 normally—incident-to billing could make that $120 instead. Over dozens of routine visits each week, the revenue boost is significant.
But here’s the catch: it’s not a free-for-all. The rules are strict, and they exist for a reason. The physician must supervise the care in very specific ways, and the patient must meet certain criteria. If you skip a step, submit a claim incorrectly, or misinterpret a rule, you could face:
· Claim denials (lost revenue)
· Audit scrutiny (time-consuming and stressful)
· Potential recoupments if Medicare decides the billing was improper
Think of incident-to like a powerful shortcut: it speeds up reimbursement and makes care more efficient, but only works if every condition is met. Skip one box, and it’s like trying to drive a car without the key—you won’t get anywhere.
Let’s say a doctor sets up a treatment plan for a patient with chronic back pain. The patient is stable and scheduled for follow-up visits every month. At the next appointment, the NP performs the visit while Dr. Patel is in the office. Because the plan was established by the doctor, the care is ongoing, and supervision rules are met, the visit can be billed incident-to, at the doctor’s rate.
Remember, incident-to billing isn’t just about money—it’s also about workflow efficiency. It allows NPs and PAs to handle routine visits without slowing down physicians, while keeping revenue optimized. But always remember: document everything. Your chart notes are your proof that every “shortcut” was followed correctly.
Key Aspects of Incident-to Billing
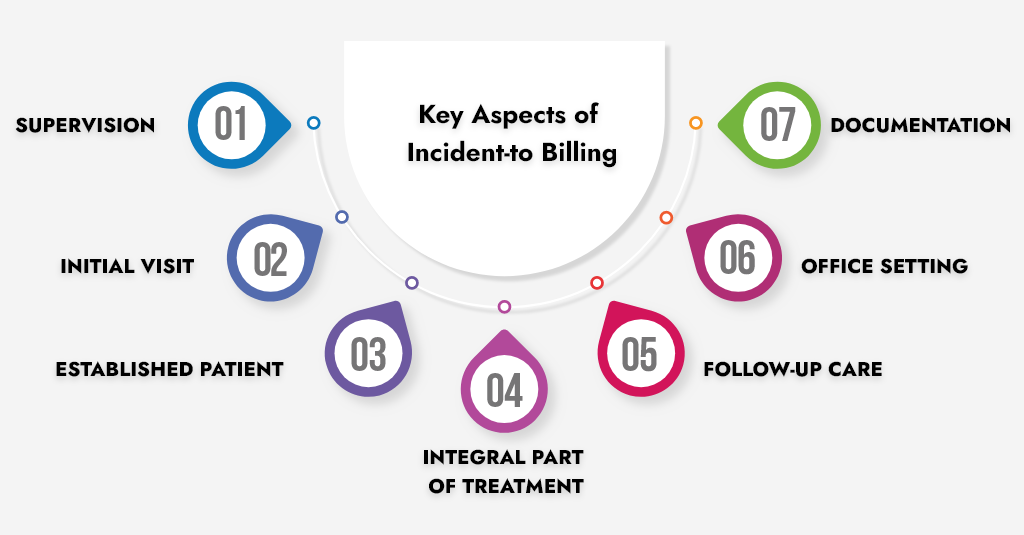
Supervision
The supervising physician must be physically present in the office suite and actively involved in the patient’s care. They don’t have to be in the same room as the NP or PA, but they must be readily available to step in, answer questions, or provide direction if needed. Think of it as being close enough to supervise in real time, not just “check-in via phone.”
For example same doctor is seeing another patient in the next exam room while the NP completes a routine diabetes follow-up. The doctor can immediately intervene if the patient develops complications—this satisfies supervision.
Initial Visit
Incident-to billing only works if the physician performed the initial visit and established the patient’s plan of care. This is the foundation—without it, subsequent visits cannot be billed incident-to.
For example, a physician diagnoses a patient with hypertension and prescribes a treatment plan. Future visits where the NP checks blood pressure or adjusts medications (within the plan) can qualify for incident-to billing.
Established Patient
The patient must already be established with the practice and have a diagnosis or condition for which the physician has initiated treatment. New patients are not eligible for incident-to billing.
For example, a patient who has been coming to your practice for routine asthma management for six months is established. Their follow-up visits with the PA can be billed incident-to.
Integral Part of Treatment
The NP/PA’s services must be integral, but incidental, to the overall treatment plan. This means the non-physician provider is carrying out a part of the care that complements the physician’s work, not performing independent or unrelated services.
Let’s say a PA performs wound care for a patient after the physician created the treatment plan—this is integral to the plan. But if the PA treats a new skin infection independently, that wouldn’t qualify.
Follow-up Care
Incident-to billing is generally used for follow-up visits, where the NP or PA is continuing the physician’s established plan of care. It’s not intended for new or complex visits.
Consider a diabetic patient who comes in for a routine lab review. The NP reviews labs, adjusts diet recommendations, and confirms the physician’s plan. That’s classic follow-up care.
Office Setting
Incident-to billing usually applies in the physician’s office or clinic (Place of Service 11). It does not apply in hospital settings, skilled nursing facilities, or other institutional settings.
For example, a PA sees a patient in your office for a follow-up hypertension check—incident-to applies. That same PA is seeing a patient in the hospital ICU? Not incident-to.
Documentation
Clear, thorough documentation is critical. The chart must show the link between the NP/PA’s service and the physician’s established plan of care. Without documentation, an audit could result in claim denials.
Tips for documentation:
· Note that the physician established the treatment plan.
· Record that the service is part of ongoing care.
· Indicate that the physician was present and supervising.
The Benefits of Incident to Billing
Incident-to billing is worth the effort because it has clear advantages:
· Higher reimbursement: You get the full physician rate instead of the NP/PA rate. That can mean thousands of extra dollars per month for routine visits.
· Better patient access: Your NPs and PAs handle routine check-ups, freeing doctors for complex cases or procedures.
· Smoother workflows: By delegating routine visits correctly, the practice runs more efficiently without compromising patient care.
It’s like setting up an assembly line—everyone does what they do best, and you get paid what you deserve.
Common Mistakes in Incident Billing
Here’s where practices often trip up:
· Billing for new patients: Incident-to only works for established patients with an existing care plan.
· The doctor isn’t on-site: No physician physically present = no incident-to.
· Major treatment changes: If the NP or PA modifies the care plan significantly, you’re out of compliance.
· Incomplete documentation: Every note must reflect that the doctor was involved, supervised the care, and approved the plan.
Best Practices For Practices and Providers
Incident-to billing can be a huge revenue saver for your practice — but only if you play by the rules and document everything properly.
Mess it up, and you’re not just risking a denial; you could be staring at refunds, audits, or even compliance headaches.
Here’s how to keep it clean, compliant, and profitable.
Train Your Team Like It’s a Group Project
Your NPs, PAs, and even your front-desk staff need to know the rules inside and out. This isn’t just for the clinicians — your schedulers and billers also need to understand when a visit can be billed incident-to and when it can’t.
Think of it this way: if any one person in the chain doesn’t get the “what, when, and how” of incident-to billing, the whole process can fall apart. Hold short training sessions, share examples of correct and incorrect billing, and make sure everyone can spot situations where incident-to isn’t allowed.
Document Like an Auditor Is Watching
Your chart note should leave no room for doubt. It needs to clearly show:
- The physician established the plan of care.
- The visit was part of ongoing care — not a brand-new problem.
- The physician was present in the office and supervising during the visit.
If you can’t point to those details in the documentation, you can’t bill it incident-to. The more specific you are, the safer you’ll be if a payer ever asks questions.
Use Templates and Prompts to Your Advantage
If you rely solely on memory, someone is going to forget a step. Build templates or checklists right into your EHR. For example, have fields that require you to document the supervising physician’s name or checkboxes to confirm this was part of an established plan. These little prompts act like safety nets, making sure you don’t miss something important before the claim goes out.
Audit Yourself Before the Payer Does
Pick a few charts each month and review them for compliance. Were all the rules met? Was the physician actually in the office? Was it part of an established care plan? By doing this regularly, you’ll catch mistakes while they’re small — and fix them before they become costly. Think of this as preventive maintenance for your revenue cycle.
Keep an Updated Playbook
Incident-to rules can change, and payers sometimes interpret them differently. Keep a quick-reference guide in your office that’s updated at least once a year (or sooner if regulations shift). This should include:
- CMS’s latest incident-to requirements.
- Payer-specific variations.
- Examples of qualifying vs. non-qualifying visits.
Having a living document like this ensures your whole team stays on the same page — literally — no matter who’s doing the billing.
Final Thoughts
Incident-to billing is a powerful tool for boosting revenue and efficiency.
Used correctly, it helps your practice run smoother, keeps patients seen on time, and increases reimbursement. Used incorrectly, it can lead to denied claims, audits, or worse.
Golden rule: Compliance isn’t optional.
Protect your practice, your staff, and your patients by doing it right. And when in doubt, consult a billing expert—it’s cheaper than fixing an audit later!
FAQs
Can I bill incident-to for a new patient?
No. Incident-to only applies to established patients who already have a treatment plan initiated by the physician. New patients always need to be billed under the provider who evaluates them first.
What counts as the doctor being “on-site” or “immediately available”?
The physician must be in the office and able to step in if needed. Being in another building, on a phone call, or working remotely does not qualify. Immediate availability means real-time supervision capability.
Can an NP or PA create a new care plan and still bill incident-to?
No. The care plan must originate with the physician. Incident-to billing is for continuing an existing plan, not starting a new one. Any significant change or new issue requires billing under the provider who initiates it.
Can temporary staff or contractors perform incident-to services?
No. Only licensed staff employed by your practice qualify. Outside contractors, locums, or visiting clinicians are not eligible.
How should I document incident-to visits?
Documentation is critical. Each note should clearly show:
· The physician established the treatment plan.
· The service was part of ongoing care.
· The physician was present and supervising.
Templates and checklists can help ensure nothing is missed.



