The world of mental health is complicated enough; the billing side shouldn’t make it worse. Yet, for many mental health professionals, getting paid for their services feels more complex than the therapy itself.
Between confusing CPT codes, payer-specific rules, and tricky documentation demands, billing can drain both time and patience.
This guide breaks it all down, so whether you’re a psychiatrist, psychologist, therapist, counselor, psychiatric NP, or clinical social worker, you’ll know exactly how to code, bill, and get reimbursed without the constant back-and-forth with payers.
Why Mental Health Billing Is Different
Unlike general medical billing, mental health billing has its own quirks. Many payers limit the number of sessions, require pre-authorizations, and apply stricter documentation standards. On top of that, most mental health visits are time-based, which makes coding accuracy crucial.
For instance, if you bill a 45-minute therapy session (CPT 90834) but document 38 minutes, you’re inviting a denial or an audit. Mental health billing demands precision — not just in coding, but in how you describe the session and time spent.
CPT Codes for Mental Health Billing

Let’s start with the bread and butter — CPT (Current Procedural Terminology) codes. These codes describe what you did during the session.
Common Mental Health CPT Codes
| Service Type | CPT Code | Description |
| Diagnostic Evaluation | 90791 | Psychiatric diagnostic evaluation (no medical services) |
| Diagnostic Evaluation w/ Medical Services | 90792 | Includes medical assessment and medication prescription |
| Psychotherapy, 30 minutes | 90832 | Individual therapy (16–37 minutes) |
| Psychotherapy, 45 minutes | 90834 | Individual therapy (38–52 minutes) |
| Psychotherapy, 60 minutes | 90837 | Individual therapy (53+ minutes) |
| Family Therapy (without patient) | 90846 | Counseling for family members |
| Family Therapy (with patient) | 90847 | Family therapy session, including the patient |
| Group Therapy | 90853 | Psychotherapy delivered in a group setting |
| Crisis Psychotherapy | 90839 | First 60 minutes of crisis intervention |
| Add-on for Crisis (each additional 30 mins) | 90840 | Used with 90839 |
Tip: Always match your documented time to the code’s time range. Even a 5-minute difference can trigger claim denials.
Psychiatry & Medication Management Codes
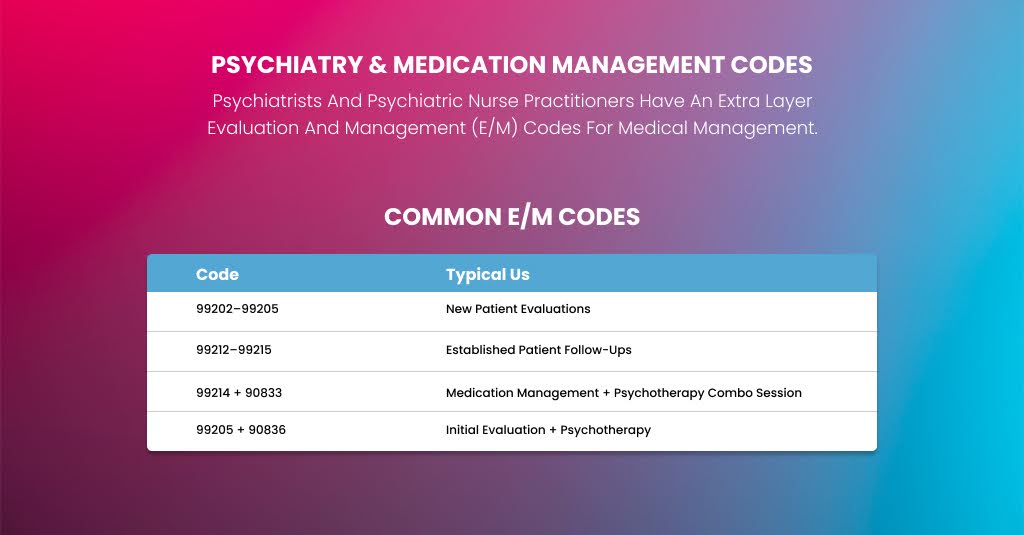
Psychiatrists and psychiatric nurse practitioners have an extra layer: Evaluation and Management (E/M) codes for medical management.
Common E/M Codes
| Code | Typical Use |
| 99202–99205 | New patient evaluations |
| 99212–99215 | Established patient follow-ups |
| 99214 + 90833 | Medication management + psychotherapy combo session |
| 99205 + 90836 | Initial evaluation + psychotherapy |
Example: A psychiatrist spends 25 minutes managing medications and 20 minutes in therapy — they’ll bill 99214 (E/M) + 90833 (psychotherapy add-on).
ICD-10 Mental Health Diagnosis Codes
Billing starts with the diagnosis. Each claim must include at least one ICD-10-CM code that matches the treatment rendered.
Most Frequently Used ICD-10 Codes:
- F32.0–F32.9 – Major depressive disorder (single episode)
- F33.0–F33.9 – Recurrent depressive disorder
- F41.1 – Generalized anxiety disorder
- F43.10–F43.12 – Post-traumatic stress disorder (PTSD)
- F31.9 – Bipolar disorder, unspecified
- F90.0–F90.9 – Attention-deficit hyperactivity disorder (ADHD)
- F20.9 – Schizophrenia, unspecified
- F50.9 – Eating disorder, unspecified
- F11.20 – Opioid dependence, uncomplicated
Make sure your documentation clearly supports the chosen diagnosis. If your note says “anxiety symptoms” but you code F41.1, you may face a denial during audit.
Documentation & Compliance Essentials
Mental health billing thrives on detailed documentation. Payers want proof that your time, diagnosis, and service type justify the code used.
Documentation Must Include:
- Patient’s presenting problem and symptoms
- Therapeutic interventions used
- Time spent in session
- Progress toward goals
- Medical necessity justification
- Signature, date, and credentials
For psychiatrists or NPs, add medication review, lab results, side effects, and treatment adjustments.
Example: “50-minute CBT session focused on reducing panic attacks. Used breathing techniques and exposure planning. Patient reports fewer episodes this week. Total time: 52 minutes.”
That’s the kind of clarity auditors and payers want.
Billing Process: Step-by-Step
Here’s the clean workflow every mental health provider should follow:
- Verify Patient Insurance & Eligibility: Check behavioral health coverage, visit limits, copays, and authorizations.
- Obtain Prior Authorization (if required): Some payers need pre-approval for therapy sessions or psychological testing.
- Document & Code Accurately: Match time, CPT, and diagnosis codes to the correct codes.
- Submit Claims Electronically: Use a clearinghouse or EHR billing module—Double-check payer-specific rules.
- Track & Handle Denials: Common denial reasons: incorrect code combos, expired authorizations, or time discrepancies.
- Post Payments & Reconcile Accounts: Verify EOBs (Explanation of Benefits) and post correctly.
- Follow Up on Unpaid Claims: Don’t let claims sit. Follow up after 30 days.
Reimbursement for Mental Health Services: What You Can Expect
Average reimbursement varies based on payer, state, and credential type.
| Service | Average Reimbursement (Medicare) |
| 90791 | $150–$180 |
| 90834 | $85–$105 |
| 90837 | $115–$140 |
| 99214 + 90833 | $150–$200 |
| 90847 (Family) | $100–$130 |
Note: Private payers often reimburse 10–30% higher than Medicare, while Medicaid typically pays lower. Always confirm your state’s Medicaid fee schedule.
Telehealth Billing for Mental Health
Telehealth changed everything for mental health practices. Most payers now cover virtual sessions with the same codes—add the appropriate modifier and place of service (POS).
Use These for Telehealth:
- Modifier 95 or GT – Indicates telehealth session
- POS 10 – Telehealth from home
- POS 02 – Telehealth from a clinic or other location
Example: A therapist conducts a 45-minute video therapy session:
90834-95, POS 10
Modifiers Commonly Used in Mental Health Billing
Modifiers provide payers with additional context about how and where you delivered care.
| Modifier | Meaning | When to Use |
| 95 | Synchronous telehealth session | Virtual sessions |
| GT | Older telehealth modifier (some Medicaid plans) | Telehealth claims |
| 59 | Distinct procedural service | To unbundle services |
| 25 | Significant, separately identifiable E/M service | When E/M and psychotherapy occur together |
| KX | Documentation on file | For medical necessity support |
Common Denials and How to Fix Them
Every mental health professional runs into denials at some point — even if everything seems correct. Most claim rejections happen because of small, technical mistakes: mismatched minutes, missing modifiers, wrong diagnosis codes, or simple authorization errors.
Below, we’ll go through the five most common mental health claim denials and how you can fix (and prevent) each one.
Denial 1: Time Mismatch Between Code and Documentation
This is one of the most frequent reasons claims get denied in psychotherapy billing.
Mental health CPT codes like 90832, 90834, and 90837 are time-based, meaning the amount of time you spend in session must align with the code you bill.
Fix:
- Always record the exact total time spent in the session — including therapy, discussion, and wrap-up.
- Match your note to the proper time range for the CPT code:
- 90832 → 16–37 minutes
- 90834 → 38–52 minutes
- 90837 → 53+ minutes
- If your sessions often run short, use 90834 instead of 90837 to avoid red flags.
Pro Tip: Auditors love clear time documentation — write “Total time spent: 54 minutes” in every note.
Denial 2: Missing or Incorrect Modifier
Modifiers are small two-character codes that explain how or where a service was provided — for example, whether it was delivered via telehealth or combined with another service.
If you forget to include the correct modifier, the payer’s system may reject or deny your claim automatically.
Example:
You conducted a 45-minute telehealth therapy session, but billed 90834 without Modifier 95. The payer thinks it was an in-person session and denies it because the place of service (POS 10 for telehealth) doesn’t match the claim type.
Fix:
- Add the correct modifier:
- 95 or GT → for telehealth services
- 25 → when billing an E/M service (like medication management) plus psychotherapy in the same session
- Double-check the payer’s rules — some Medicaid plans still use GT, while most commercial payers now prefer 95.
Denial 3: Non-Covered Diagnosis
Sometimes your claim gets denied not because of your coding, but because the diagnosis you billed isn’t covered under the patient’s plan.
Example:
You bill F43.20 (Adjustment disorder, unspecified) for therapy, but the patient’s plan only covers F32 (Major depressive disorder) or F41 (Anxiety disorders) under behavioral health benefits.
The claim is denied as a “non-covered diagnosis.”
Fix:
- Always cross-check the diagnosis with the payer’s behavioral health coverage list before billing.
- If a diagnosis isn’t covered, but treatment is clinically necessary, submit an appeal with detailed progress notes and a letter of medical necessity.
- For ongoing therapy, update the diagnosis if symptoms evolve and justify it in your documentation.
Tip: Avoid “unspecified” ICD-10 codes (like F41.9 or F32.9) when possible — payers prefer specific, clearly supported diagnoses.
Denial 4: No Prior Authorization
Many insurance plans — especially Medicaid and certain commercial carriers — require pre-authorization before you begin therapy or psychological testing. Skipping this step almost guarantees a denial.
Example:
You start therapy sessions without checking if the plan requires prior authorization after the initial evaluation. After 10 sessions, you submit claims, and all are denied as “no prior authorization on file.”
Fix:
- Before the first session, verify:
- Does the plan require pre-authorization?
- How many sessions are covered?
- Is there a cap or renewal process after a certain number?
- If authorization wasn’t obtained, appeal using clinical documentation showing why the sessions were medically necessary.
- Keep track of authorization expiration dates and renew on time.
Pro Tip: Many clearinghouses or EHRs let you set reminders for expiring authorizations — use them religiously.
Denial 5: Duplicate or Bundled Services
Duplicate denials happen when you accidentally bill the same service twice on the same day, or when two codes you billed are considered “bundled” under payer rules.
Example:
A psychiatrist bills both 90833 (psychotherapy add-on) and 90834 (standalone psychotherapy) in one claim. The payer considers that duplicate because 90833 is meant to be an add-on to an E/M code, not a separate therapy session.
Fix:
- Review your coding combinations. If you provided E/M + psychotherapy, use 99214 + 90833, not 90834.
- When two procedures are truly separate (e.g., group therapy and individual therapy on the same day), use Modifier 59 to indicate they were distinct sessions.
- Include time documentation and a clear description of why both services were necessary.
| Best Practices for Mental Health Practices and Providers – Use mental health-friendly EHRs like SimplePractice, TherapyNotes, or Valant. – Stay credentialed with all major payers — credentialing delays can cost months of lost revenue. – Review EOBs weekly to catch underpayments early. – Keep session notes compliant — payers often request chart reviews. – Educate your front desk staff to verify coverage before scheduling. – Offer self-pay options with transparent rates to avoid unpaid balances. |
Final Thoughts
Mental health professionals spend their days healing others, but getting paid shouldn’t be a battle. Once you understand how CPT codes, modifiers, and payer rules fit together, billing becomes far less intimidating.
This guide is like your roadmap — whether you’re a solo therapist in private practice or part of a behavioral health group, follow these best practices, and you’ll not only get reimbursed faster but also stay fully compliant and audit-ready.
Increase Your Mental Health Revenue with A2Z Billing
Your mental health expertise deserves reliable revenue—not billing headaches. Let A2Z Medical Billing Experts in New York handle your coding, claims, and reimbursements while you focus on what truly matters: your patients.
Most practices see a 20–40% increase in collections within 90 days of switching to professional billing support.



