Get home health billing revenue cycle management services powered by an advanced AI-powered home health billing company. A2z Medical Billing Solutions helps healthcare providers manage challenges that damage their practice’s earnings. We help physicians with timely and error-free billing and coding, improving efficiency to stop revenue leakages.
A2Z medical billing experts offer the best home health billing solutions in New York and across the US. We have been serving the home health practices for the last 10+ years, resulting in maximum collections, timely Medicaid submissions and payment posting, shorter turnaround times, and fewer claim denials.
Our home health revenue cycle management team understands the nature of challenges a medical practice faces every day in the US. For a streamlined medical billing process, you require specialized knowledge and constant updates that only we can offer reliably and economically. We help healthcare organizations, including clinics, hospitals, and labs, to reduce in-house billing errors and improve their quality-driven work by two-fold. Over 400 home health agencies across the US trust our teams in optimizing their revenue with minimal disruptions to their cash flow.


Home health billing services involve the process of generating claims and submitting them to insurance payers for medical care offered by home health agencies to patients at their homes. The billing process for such medical care services is complex, involving multiple steps, including the OASIS assessment, eligibility checks, generating Medicare claims according to payer policies, timely submissions, and collecting patient payments.
Due to the complexities of home health coding and billing, as well as the lengthy steps involved in verifying benefits eligibility from Medicare’s HETS database, outsourcing enables healthcare providers to submit Medicare claims in accordance with payer requirements and minimize the number of unbilled claims.
We streamline the billing process for home health agencies and practices, freeing providers to focus solely on patient care and improving quality of life.
Outsourcing increases operational efficiency by double, allowing better denial management, error-free home health billings, and Medicaid submissions.
Home health billing offers unique and complex challenges at every step, and overcoming them is essential for lowering claim denials. The common challenges home healthcare providers face are
Home health agencies have to tackle various regulations and payer-specific requirements, especially Medicare and state-specific Medicaid rules. Non-compliance results in penalties and fines for providers in the US.
Inconsistent or missing documentation results in front-end denials and increasing aging account receivable cases. A new or untrained in-house clinical team increases documentation mistakes, directly affecting your revenue cycle
Complex coding for home health medical services requires complete knowledge of ICD-10-CM, CPT, and HCPCS codes. Using invalid or outdated home health codings increases claim denials.
Understanding of claim filing deadlines is important to prevent late submissions. The majority of Medicare claims are rejected due to non-compliance with time and format requirements.
Besides offering the industry’s most advanced home health billing solutions, we also provide help to healthcare practices in getting credentialed and enrolling with government and commercial insurers. Our comprehensive home health revenue cycle management services include:
Prompt and comprehensive eligibility verification of patients to determine home health benefits they are eligible for, and taking prior authorization if required by the payers in advance to enhance cash flow and shorten the turnaround time
We offer accurate and compliant coding and billing solutions to home health agencies with electronic claim submissions. Each patient’s file data is thoroughly analyzed, including provider notes, diagnostic reports, and accurate ICD, CPT code is applied.
Our medical billing team diligently pursues aging ARs to recover the owed amount from patients and insurance payers. All past dues are categorised, and various communication channels are used, like email, mail, calls, and texts, to recover reimbursement.
We help new and established medical practices with credentialing and provider enrollment programs. We thoroughly assist healthcare providers in CAQH profile maintenance, payer setup, patient payments, to signing contracts for in-network and out-of-network enrollment selections.

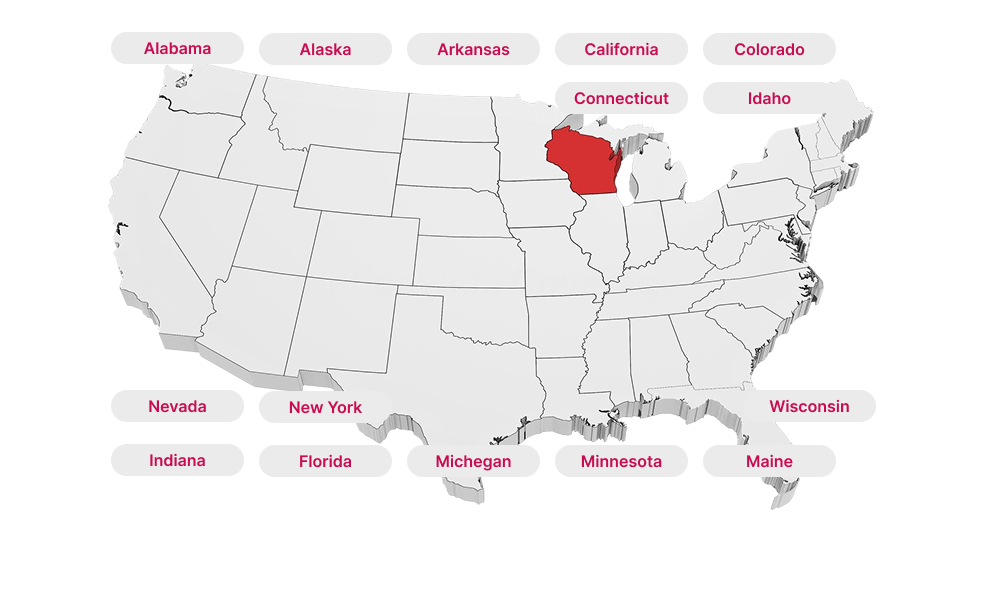
At AR home health billing company, we offer state-of-the-art medical billing services across all 50 states of the US. By hiring our RCM experts, medical practices may achieve the following results:


Our home health revenue cycle management team has expertise in working with different commercial and government payers, including:


We provide periodic financial performance reporting and analytics to ensure best practices are followed across all healthcare organizations. Our proactive approach helps providers in:
Our AI-powered medical billing software allows claim automation, freeing your team from time-consuming work to improve patient care with ease. We offer easy integration with the existing EHR/EMR system you’re using, with real-time access to digital workflows, amplifying the effect of claim submissions and strengthening financial health. We have a good command of various billing software, including: