If you’re a physical therapist, occupational therapist, or speech-language pathologist, you’ve probably wrestled with Medicare’s 8-minute Rule more times than you’d like to admit.
At first glance, it sounds simple: spend at least eight minutes providing a therapy service, and you can bill one unit. Easy, right?
Not quite.
Between timed codes, untimed codes, remainders, modifiers, and payer-specific variations, the 8-minute Rule has tripped up countless therapy practices. One missed detail can cost you hundreds in denied claims—or worse, trigger a compliance audit.
So let’s unpack it all step by step and provide practical advice you can actually use.
What Is Medicare’s 8-Minute Rule?
The 8-minute Rule is a Medicare billing guideline for timed therapy services under Part B (outpatient therapy). It tells you how to convert total treatment minutes into billable units using 15-minute increments.
In simple terms:
If you spend at least 8 minutes providing a direct, one-on-one, skilled therapy service, you can bill one unit of that CPT code.
Each “unit” represents 15 minutes of treatment, but Medicare allows partial units once you hit that 8-minute threshold.
Let’s look at the official Medicare timetable:
| Total Timed Minutes (All Services Combined) | Billable Units |
| 8–22 minutes | 1 unit |
| 23–37 minutes | 2 units |
| 38–52 minutes | 3 units |
| 53–67 minutes | 4 units |
| 68–82 minutes | 5 units |
| 83–97 minutes | 6 units |
This is straight from the Medicare Claims Processing Manual (Chapter 5, Section 20.2) — the gold standard reference every therapist should bookmark.
Timed vs. Untimed Codes: Know the Difference Before You Bill
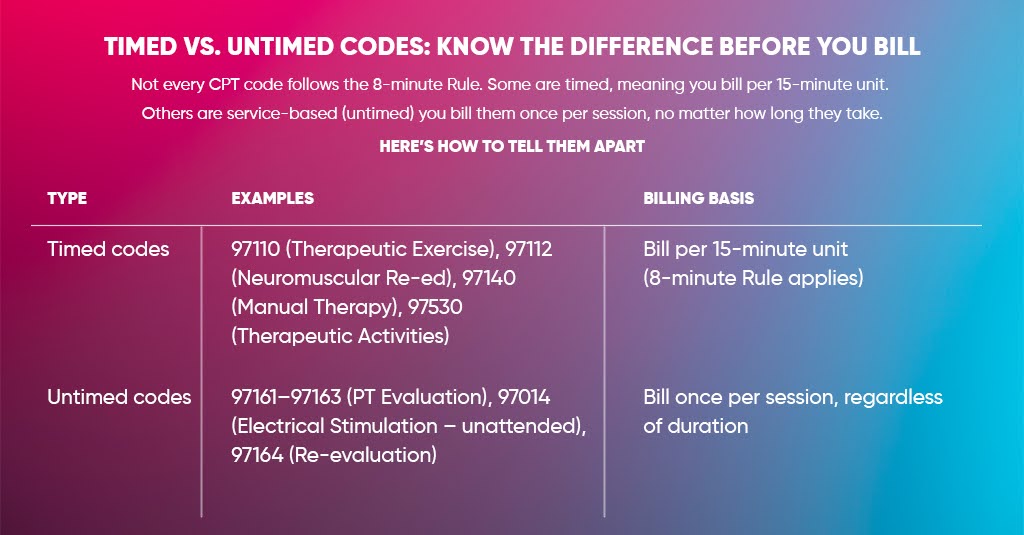
Not every CPT code follows the 8-minute Rule.
Some are timed, meaning you bill per 15-minute unit. Others are service-based (untimed) — you bill them once per session, no matter how long they take.
Here’s how to tell them apart:
| Type | Examples | Billing Basis |
| Timed codes | 97110 (Therapeutic Exercise), 97112 (Neuromuscular Re-ed), 97140 (Manual Therapy), 97530 (Therapeutic Activities) | Bill per 15-minute unit (8-minute Rule applies) |
| Untimed codes | 97161–97163 (PT Evaluation), 97014 (Electrical Stimulation – unattended), 97164 (Re-evaluation) | Bill once per session, regardless of duration |
The 8-minute Rule only applies to timed codes. Untimed codes are billed once per day, even if you spend 45 minutes on them.
How the 8-Minute Rule Works
The 8-minute Rule determines how many units you can bill for timed therapy services under Medicare Part B. It doesn’t care how many different CPT codes you use — it cares how much total time you spent providing one-on-one, skilled therapy.
Think of it as a math formula with three key steps:
- Add up all the timed minutes you spent.
- Match that total to Medicare’s unit table.
- Distribute those units to the codes that took the most time.
Let’s break this down with practical examples.
Step 1: Add Up All the Timed Minutes
First, list every timed CPT code you used during that session and note exactly how many minutes you spent on each.
Here’s an example:
| CPT Code | Description | Time Spent |
| 97110 | Therapeutic Exercise | 15 min |
| 97140 | Manual Therapy | 10 min |
| 97530 | Therapeutic Activities | 12 min |
Total Timed Minutes = 15 + 10 + 12 = 37 minutes
Step 2: Match the Total to Medicare’s Time Table
Now, take those 37 minutes and check them against the official Medicare 8-minute table:
| Total Timed Minutes | Billable Units |
| 8–22 minutes | 1 unit |
| 23–37 minutes | 2 units |
| 38–52 minutes | 3 units |
| 53–67 minutes | 4 units |
| 68–82 minutes | 5 units |
| 83–97 minutes | 6 units |
Your total (37 minutes) falls into the 23–37 range, which means you can bill 2 units total.
Step 3: Assign Units to Each Code
Now comes the part where most people mess up — how to split those two units between multiple codes.
The Rule is simple:
Assign one unit to the service that took the most time first, then use the remaining time for the next service.
In our example:
- 97110 (Therapeutic Exercise): 15 minutes
- 97530 (Therapeutic Activities): 12 minutes
- 97140 (Manual Therapy): 10 minutes
Since 97110 took the most time, it gets the first unit.
The remaining 22 minutes (12 + 10) qualify for the second unit.
Final Billing:
- 1 unit of 97110
- 1 unit of 97530 (or 97140 — whichever fits the treatment rationale better)
Step 4: Handle Leftover Minutes (The “Remainder” Rule)
Now, let’s say you had a slightly different scenario:
| Code | Minutes |
| 97110 | 20 |
| 97530 | 13 |
| Total | 33 minutes |
33 minutes also lands in the 23–37 range, so you get 2 units total.
But what if you had 38 total minutes?
Now you’ve entered the 38–52 range, which equals 3 units.
The secret is in the remainder:
- After billing whole 15-minute chunks, count the leftover minutes.
- If the remainder is 8 minutes or more, it’s billable as an extra unit.
- If it’s 7 or less, it’s not.
Example:
- 15 + 15 + 8 = 38 → 3 units
- 15 + 15 + 7 = 37 → 2 units only
That one minute can make a difference between getting paid for 2 units or 3.
Step 5: Only Count Skilled, Direct, One-on-One Time
This part is critical for compliance.
Only count direct, skilled, face-to-face time that involves active therapy intervention. Do not include:
- Rest breaks
- Setup or clean up
- Patient education outside of active treatment
- Documentation time
- Unsupervised exercise or unattended modalities
Example:
You spend 5 minutes setting up an exercise machine and 10 minutes actually supervising the patient.
→ Only the 10 minutes count toward the 8-minute Rule.
| Example With Multiple Codes and RemaindersLet’s do a more complex case.CodeMinutes97110 (Therapeutic Exercise)2297140 (Manual Therapy)797530 (Therapeutic Activities)9Total Timed Minutes3838 minutes = 3 units total.Now assign:1st unit → 97110 (longest time: 22 min)Remaining 16 minutes (7 + 9) → qualify for 2 more units combined.Final:97110 → 1 unit97140 → 1 unit97530 → 1 unitAltogether, 3 total units were billed correctly. |
What Happens if the Total Time Is Below 8 Minutes?
If your total timed minutes for the day (across all timed codes) is less than 8 minutes, you cannot bill for any timed unit.
Medicare expects at least 8 minutes of direct skilled intervention to justify one unit.
Example:
- 97110 = 5 minutes → No billable unit.
Medicare’s Golden Formula for Quick Calculations
If you want to remember this quickly during your day:
Total timed minutes ÷ 15 = Number of full units
If remainder ≥ 8 → Add 1 more unit
If remainder ≤ 7 → Don’t add
Example:
43 total minutes ÷ 15 = 2 full units (30 min), remainder = 13 → Bill 3 units.
41 minutes ÷ 15 = 2 full units, remainder = 11 → Still 3 units.
37 minutes ÷ 15 = 2 full units, remainder = 7 → Only 2 units.
How to Handle Leftover Minutes (The Remainder Rule)
Here’s where people slip up.
Let’s say you provided:
- 20 minutes of 97112 (Neuromuscular Re-education)
- 13 minutes of 97530 (Therapeutic Activities)
Total = 33 minutes.
33 minutes also falls in the 23–37 range, so you get 2 units total.
Now, here’s the Rule for leftovers:
- Add up all timed minutes.
- Subtract whole 15-minute chunks.
- If the remainder is 8 or more minutes, you can bill an extra unit.
- If it’s 7 or less, you can’t.
So if your total were 38 minutes (15 + 15 + 8), you’d qualify for three units.
Medicare says you can combine leftover minutes across different timed services, as long as the total remainder is ≥ 8.
Documentation: The Secret to Surviving Medicare Audits
Medicare won’t just take your word for it. They need proof.
Your documentation should clearly show:
- Start and stop times (or total timed minutes)
- Services performed (CPT code + description)
- Patient’s response and progress
- Functional goals related to each service
- Signatures of the treating provider
Example entry:
97110 – 15 min: TherEx for upper extremity strengthening using resistance bands.
97140 – 10 min: Manual therapy – soft tissue mobilization of right shoulder.
Total Timed: 25 min (2 units). Patient tolerated treatment well with improved mobility.
Never include setup, rest, or documentation time in your total. Only direct, skilled, face-to-face time counts.
The 8-Minute Rule vs AMA CPT Rule (They’re Not the Same)
A significant point of confusion: not all payers use the same time calculation method.
| Criteria | Medicare 8-Minute Rule | AMA CPT Midpoint Rule |
| What It Measures | Total combined time for all timed codes | Time spent per individual code |
| Billing Unit Threshold | ≥ 8 minutes of total remaining time | ≥ 8 minutes of each 15-minute code |
| Used By | Medicare Part B, some Medicare Advantage plans | Commercial insurers, Tricare, etc. |
So, if you’re billing Cigna, Aetna, or BCBS, check their provider manual first. Many private payers follow the AMA midpoint rule, not Medicare’s total-time method.
When the 8-Minute Rule Doesn’t Apply
- Untimed codes (evaluations, re-evaluations, group therapy)
- Concurrent therapy (multiple patients at once)
- Modalities without constant attendance
- Non-Medicare payers following the CPT midpoint method
- Facility-based services (like SNFs, home health), where different rules may apply
Special Modifiers You Must Know
Medicare requires therapy-specific modifiers for proper claim routing:
| Modifier | Used For |
| GP | Physical Therapy |
| GO | Occupational Therapy |
| GN | Speech Therapy |
| CQ | Services furnished in part or whole by a Physical Therapist Assistant (PTA) |
| CO | Services furnished in part or whole by an Occupational Therapy Assistant (OTA) |
If a therapy assistant provides part of the treatment, you must determine whether the therapist contributed enough to meet the 8-minute threshold for the final unit. If not, the CQ/CO modifier applies — and reimbursement may be slightly reduced.
Best Practices for Therapy Practices
Here’s how smart clinics stay compliant and efficient:
- Use digital timers or EMR auto-tracking for each session.
- Plan treatment blocks strategically — avoid finishing at 7 minutes.
- Train staff quarterly on Medicare updates and payer differences.
- Keep a cheat sheet (like the table above) visible near treatment stations.
- Document clearly: “timed” vs “untimed” sections separated in your notes.
- Audit 5 random charts per month to ensure your billed units match the minutes.
- Stay updated: CMS updates therapy billing rules annually in the Physician Fee Schedule.
Final Thoughts
Medicare’s 8-minute Rule might look like simple math, but it’s more like a billing equation with compliance consequences. One miscounted minute, one unchecked modifier, or one wrong code allocation — and you’re looking at delayed payments or audit flags.
Think of it this way:
“If it isn’t timed, it isn’t billable. If it isn’t documented, it didn’t happen.”
Stay sharp, stay consistent, and train your team to treat time as data — because in therapy billing, every minute truly counts.
Want to simplify this entire process?
Partner with A2Z Medical Billing Services, a billing team that specializes in therapy coding and Medicare compliance.
We offer physical therapy billing services in the USA and handle every step from coding and modifiers to claim submission and audit defense.
Schedule a free RCM review.
FAQ 1
Does the 8-minute rule apply to each CPT code separately?
No. Medicare applies the 8-minute rule to the total combined time of all timed therapy services, not per individual CPT code.
FAQ 2
Can leftover minutes from different CPT codes be combined?
Yes. Medicare allows combining leftover minutes across timed codes as long as the total remainder is 8 minutes or more.
FAQ 3
Does Medicare Advantage follow the 8-minute rule?
Not always. Some Medicare Advantage plans follow the AMA midpoint rule. Always verify payer-specific guidelines.
FAQ 4
What documentation is required to support 8-minute rule billing?
Clear total timed minutes, services performed, patient response, functional goals, and provider signature are required.
FAQ 5
What happens if therapy assistants provide part of the service?
Modifiers CQ (PTA) or CO (OTA) may apply, potentially reducing reimbursement if assistant time exceeds allowed thresholds.



