If you’ve ever opened an insurance denial for Acute Kidney Injury (AKI), you know the frustration. It’s a common scenario, and many of these denials link back to one code: N17.9.
This code—”Acute Kidney Injury, unspecified”—serves a purpose in billing. Yet it’s frequently applied incorrectly, leading to payment delays and revenue loss.
This guide provides a straightforward overview of N17.9. We’ll clarify when it’s appropriate to use, when it isn’t, and how documentation affects your claims.
The Acute Kidney Injury Coding Gray Zone
Consider N17.9 (“Acute kidney injury, unspecified”) as your safety net. It’s the code you use when you know the Patient has AKI – the doctor said it, the labs support it – but the crucial details are missing. Specifically, it means:
The AKI is confirmed: The provider explicitly documented “Acute Kidney Injury,” “AKI,” or sometimes “Acute Renal Failure” (though AKI is the preferred term).
Why is it unclear?
Because the chart doesn’t state a clear cause, was it dehydration? Sepsis? A toxic drug reaction? N17.9 says, “We don’t know yet.”
The how bad is unclear:
The provider didn’t assign a stage (Stage 1, 2, or 3) using recognized criteria, such as KDIGO (Kidney Disease: Improving Global Outcomes).
N17.9 isn’t lazy coding; it’s honest coding when the documentation genuinely lacks Specificity.
Studies show that up to 30% of N17.9 usage could potentially be coded more specifically if documentation were clearer.
That presents a significant opportunity for improvement.
When N17.9 is Your Only Option (And When It’s a Red Flag)
Use N17.9 confidently ONLY in these scenarios:
The Acute Kidney Injury Diagnosis is Solid, But Details Are Absent: The provider clearly states AKI, but the record is silent on cause and stage. You cannot assume or infer.
Example: A patient presents with elevated creatinine. The doc notes “Acute Kidney Injury” and orders fluids, but hasn’t documented the suspected cause (e.g., “likely dehydration”) or staged it yet. N17.9 is appropriate at that moment.
Initial Presentation, Workup Pending: Sometimes, AKI is identified early, and the full diagnostic workup (to determine the cause and stage) is not yet complete. N17.9 might be used briefly here. But this is temporary.
As soon as more info is available (often within 24-48 hours), you should update the code if possible.
AVOID N17.9 Like the Plague If:
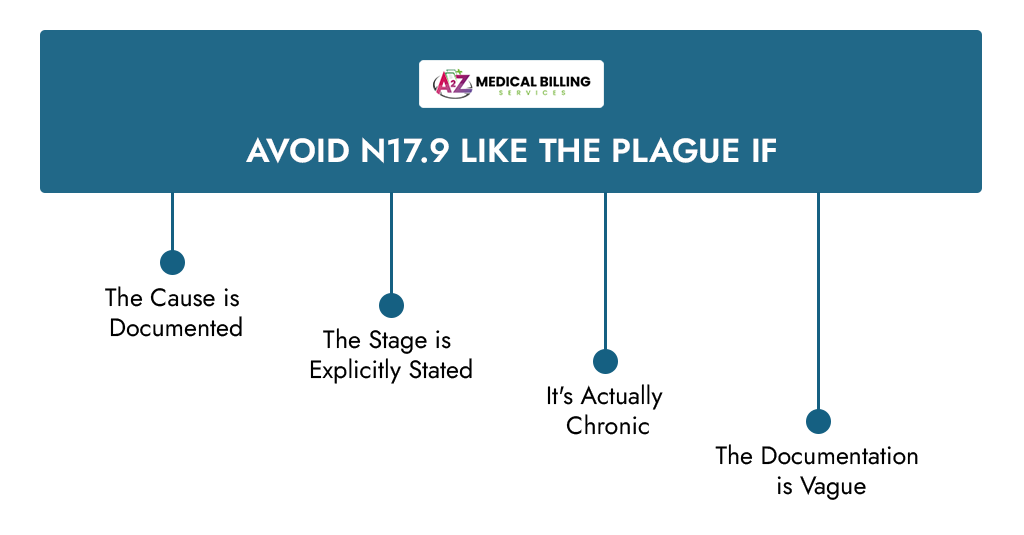
- The Cause is Documented: If the note says ” Acute Kidney Injury secondary to severe dehydration,” using N17.9 is a denial waiting to happen. You need the code for dehydration (E86.0) plus the appropriate AKI code. While N17.9 might still be used if the stage isn’t documented, always prioritize the cause first. Payers see a missing cause as a lack of medical necessity.
- The Stage is Explicitly Stated: This is non-negotiable. If the chart reads “AKI Stage 2,” you MUST use N17.2. Using N17.9 here screams “incorrect coding” to auditors. Stat Alert: Claims using non-specific AKI codes (such as N17.9) when a specific stage is documented have denial rates exceeding 25%, according to some payer analyses.
- It’s Actually Chronic: AKI is sudden. CKD (Chronic Kidney Disease) is a long-term condition. Using N17.9 for CKD (or vice versa) is a fundamental error. CKD codes start with N18. Mixing these up is a top audit trigger.
- The Documentation is Vague: “Renal failure,” “kidney dysfunction,” or “elevated BUN/Cr” are NOT diagnoses of AKI. They are findings. You need the provider to state “Acute Kidney Injury explicitly. Payers reject claims based solely on lab abnormalities without a clear, linked diagnosis.
The Documentation Requirements for Acute Kidney Injury
Your reimbursement hinges entirely on what the provider writes. Coders aren’t mind readers. Here’s the gold you need to unearth in those notes:
- The Explicit AKI Diagnosis: Look for the words “Acute Kidney Injury” or “AKI.” “Acute Renal Failure” is often accepted as synonymous, but AKI is preferred. Without this, you can’t code AKI at all.
- The Cause (Etiology): This is HUGE. Knowing why the AKI happened provides a medical necessity for tests and treatments. Look for phrases like:
It links the Acute Kidney Injury to other conditions or procedures, justifying the resources used. A specific cause often supports a higher level of service.
- The Stage (Severity): Staging (1, 2, or 3) directly correlates with severity, treatment intensity (like dialysis), and prognosis. Look for:
- “AKI Stage 1” (N17.1)
- “AKI Stage 2” (N17.2)
- “AKI Stage 3” (N17.3)
- Stage is a key indicator of severity. Higher stages often require more complex and costly care. Using N17.9 for a Stage 3 AKI significantly under-represents the Patient’s condition and can lead to underpayment or denial for associated services (like dialysis).
- Confirmation of Acuity: Ensure the context makes it clear this is a new, acute problem, not a worsening of known CKD. Look for timelines (“new onset,” “sudden rise in creatinine”).
Don’t just passively read.
If details are missing, send a quick, specific query to the provider while the encounter is fresh. Example: “Patient diagnosed with AKI. Please clarify:
- Suspected cause?
- Is AKI stage determinable per KDIGO criteria?
This ensures accurate billing.
Practices that implement structured query templates see a reduction of up to 40% in AKI coding denials.
The Payer Perspective: Why Specificity is Your Reimbursement Superpower
Insurance companies aren’t being difficult just for the sake of it. They need specifics to:
- Validate Medical Necessity: A vague N17.9 doesn’t tell them why the AKI happened or how severe it is. A specific code like N17.2 (Stage 2) linked to E86.0 (Dehydration) paints a clear picture: “This patient was severely dehydrated, causing significant kidney damage requiring intervention.” That’s justifiable. N17.9 alone? It raises questions.
- Assess Risk and Cost: Specific codes (especially higher stages) help payers understand patient complexity and predict costs. This is crucial in value-based care models. Payers are aware that unspecified codes, such as N17.9, are sometimes used to “upcode” or when documentation is inadequate. They scrutinize them heavily. Over-reliance on N17.9 can flag your practice for audits. Data shows that practices with high rates of unspecified codes face three times more audit requests.
- Prevent Fraud and Abuse: Consistent, vague coding can be a red flag for potential overbilling. Specificity demonstrates transparency and accurate reporting.
- Process Claims Faster: Clear, specific codes with supporting documentation mean fewer edits, fewer manual reviews, and faster payment. Stat: Claims using the most specific AKI codes (N17.1-N17.8) with documented cause/stage are paid, on average, 12-15 days faster than those relying solely on N17.9 (MGMA data).
A Strong Billing Strategy for Practices and Providers
Using N17.9 correctly is step one. Here’s how to build a system that minimizes its use and maximizes reimbursement:
- Prioritize Specificity First: Make it a mantra for coders: “Find the cause. Find the stage. Only use N17.9 if they are truly absent.”
- Empower Providers: Educate them on the importance of specific documentation. Show them examples of good vs. poor notes. Explain how it directly impacts payment and reduces their own administrative burden from denials. Provide templates or checklists for AKI documentation prompts.
- Implement Proactive Querying: Don’t wait for the claim to be denied. Build query processes into your workflow for common AKI documentation gaps. Aim to query within 3 days of the encounter.
- Leverage Technology: Use your EHR’s tools. Can you create smart phrases that prompt providers to select the cause/stage when they choose “AKI”? Can coders set up flags for encounters with Acute Kidney Injury diagnoses that lack Specificity?
- Track and Analyze Denials: Don’t just resubmit. Categorize every AKI denial: Was it a missing cause? Missing stage? Incorrect code (N17.9 used when a specific available)? Use this data to target education and process improvements. A medium-sized practice losing just 5 AKI claims per month due to N17.9 issues could be losing over $ 25,000 annually in delayed or denied revenue.
- Know Your Payers: Although the rules are based on ICD-10, some payers have specific Local Coverage Determinations (LCDs) or policies regarding AKI coding, particularly for dialysis or particular causes. Stay informed.
The Bottom Line
N17.9 is vital for those moments when AKI is real, but the details aren’t yet available. But it should never be your default. Think of it as the “chameleon code” – it adapts to the lack of information, but it shouldn’t be the primary color of your AKI billing picture.
Your path to faster payments and fewer denials is paved with Specificity: relentless pursuit of clear cause and stage documentation, smart querying when details are missing, and using the most precise code possible every single time.
Mastering this distinction – knowing when N17.9 is honest and when it’s a hazard – transforms your AKI billing from a source of frustration into a streamlined, revenue-protecting machine. Now hunt for that documentation gold!
FAQS?
When is it appropriate to use N17.9?
Use N17.9 only when:
- Acute Kidney Injury is explicitly documented (not just elevated creatinine)
- Cause is not stated (e.g., no dehydration, sepsis, or medication link)
- Stage (1/2/3) is undocumented
- It’s the initial encounter before the workup is completed.
Always verify documentation first—this code is for true unknowns.
If the doc notes “AKI likely due to dehydration,” can I use N17.9?
No. Documented causes (e.g., dehydration, sepsis) require coding the cause plus the most specific Acute Kidney Injury code possible. N17.9 ignores the known cause, triggering denials. Always prioritize the documented etiology.
What’s the biggest N17.9 mistake leading to denials?
Using N17.9 when the AKI stage is documented (e.g., “Stage 2”). If the note specifies a stage, you must use the matching code (e.g., N17.2 for Stage 2). This error alone causes more than 25% of AKI denials.
How can providers efficiently document the cause/stage of AKI?
- Simplify education: Show 1-line examples of clear vs. vague notes.
- Use EHR prompts: Auto-ask “Cause?” and “Stage?” when AKI is selected.
- Send targeted queries: Ask for only missing details (e.g., “Please specify AKI stage”).
- Share denial costs: Anonymized examples of revenue lost to vague notes.
Why do AKI (N17) vs. CKD (N18) coding errors cause denials?
Acute Kidney Injury is sudden/potentially reversible; CKD is chronic/progressive. Using N17.9 for CKD (or vice versa) is a diagnostic mismatch. Payers deny because the code does not accurately reflect the clinical reality or treatment needs.
Does correct N17.9 use guarantee payment?
No. Even when accurate, N17.9 claims often face:
- Closer payer scrutiny (slower processing)
- Potential underpayment if severity is undercoded
- Higher denial risk vs. specific AKI codes (N17.1-N17.8).
What’s the financial cost of AKI coding errors?
Beyond denied claims:
- Rework costs: $25–50+ per denial in staff labor
- Cash flow delays: Payments stalled 60–90+ days
- Audit risk: High N17.9 use flags practices for reviews
- Annual loss: Up to $30K for 5 monthly denials (direct costs + rework + delays). Accurate coding protects revenue.



